Key Takeaways:
- Malabsorptive bariatric surgeries work by limiting the number of calories and nutrients your body absorbs from food.
- These procedures typically result in greater weight loss compared to purely restrictive surgeries, such as the gastric sleeve.
- While highly effective, malabsorptive surgeries require lifelong vitamin supplementation and regular monitoring to prevent serious nutritional deficiencies.
If you're exploring weight loss surgery options, you've probably come across terms like "restrictive" and "malabsorptive" procedures. While restrictive surgeries primarily limit how much food you can eat, malabsorptive bariatric surgery works differently. They change how your body absorbs nutrients. For some people struggling with severe obesity, this approach can be life-changing. It has also shown promise in addressing bariatric surgery and diabetes, bariatric surgery for hypertension, and bariatric surgery for GERD (gastroesophageal reflux disease).
But what exactly is malabsorptive bariatric surgery, and could it be the right choice for you? We'll break down these powerful but complex procedures into simple, straightforward information that will help you understand your options.
[/box]
Types of Malabsorptive Bariatric Surgeries
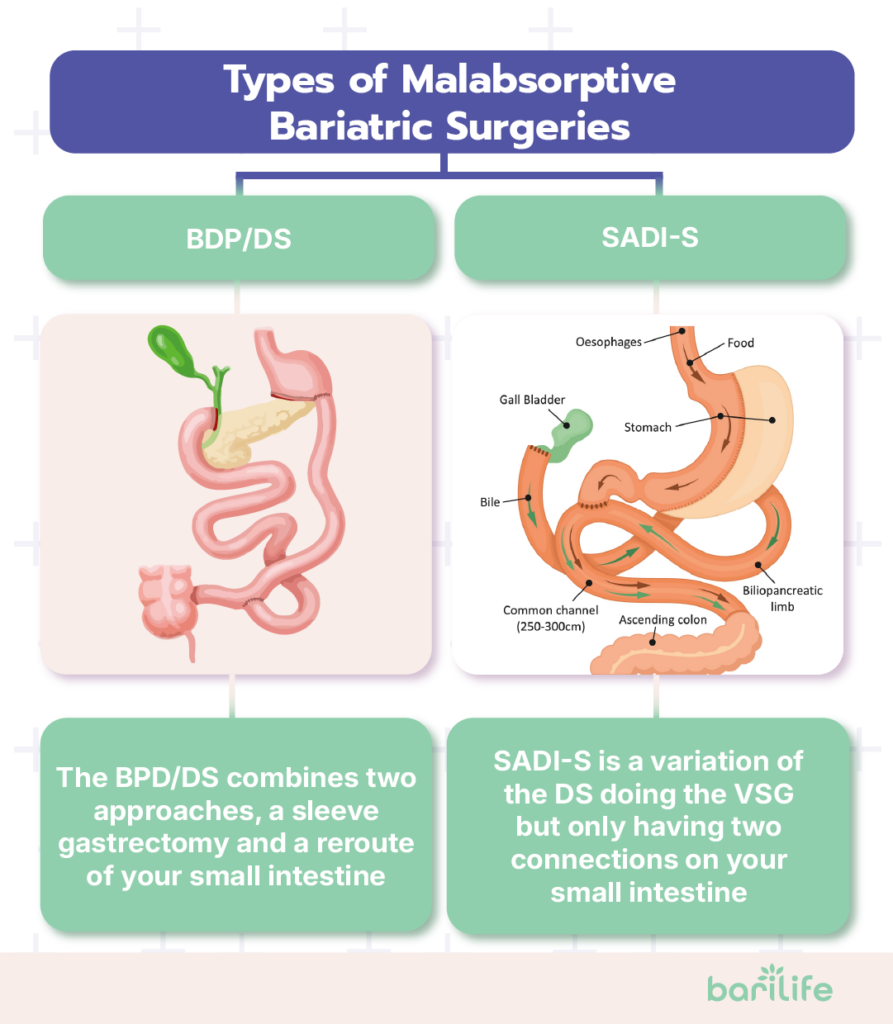
When we talk about bariatric surgeries, restrictive malabsorptive procedures are considered among the most powerful options available. Let's look at the main types:
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
This procedure, despite its long name, actually has a pretty straightforward concept. The BPD/DS combines two approaches:
First, surgeons remove about 70% of your stomach, creating a smaller, sleeve-shaped stomach (similar to a sleeve gastrectomy).
Second, and this is where the malabsorptive part comes in, they reroute your small intestine. Food bypasses most of your small intestine, where most nutrient absorption occurs. Meanwhile, digestive juices from your pancreas and bile don't mix with food until the final section of your small intestine.
Think of it as shortening the path that food takes through your body, giving it less time to be absorbed. The result? You absorb significantly fewer calories and nutrients from the food you eat.
This is one of the most powerful malabsorptive bariatric surgery examples, but it also requires the most significant lifestyle adjustments afterward.
Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
The SADI-S is a newer, simplified variation of the duodenal switch. It begins with creating a sleeve gastrectomy, which involves removing part of the stomach. Then, instead of creating multiple connections in your intestines, surgeons make just one connection between your duodenum (the first part of your small intestine) and your ileum (the last part).
This single-connection approach makes the surgery technically simpler and potentially reduces complications, while still providing effective treatment for malabsorption. You'll still absorb fewer nutrients and calories, but the procedure is less complex than a traditional duodenal switch.
Roux-en-Y Gastric Bypass (RYGB)
The gastric bypass is probably the most well-known procedure that combines restrictive and malabsorptive bariatric surgery elements. Here's how it works:

Surgeons create a small stomach pouch, approximately the size of an egg, which drastically limits the amount of food that can be eaten at once (the restrictive part).
Then, they connect this pouch directly to the middle part of your smaller intestine, bypassing the rest of your stomach and the first part of your small intestine.
This bypass means you'll absorb fewer calories and nutrients from food. However, the degree of malabsorption is less than with BPD/DS or SADI-S procedures, making it a more moderate option.
How Malabsorptive Bariatric Surgery Works
To understand if these surgeries might be right for you, it helps to know exactly how they work to promote weight loss. There are three main mechanisms:
Reduction of Absorptive Surface Area
The primary way malabsorption bariatric surgery works is by reducing the amount of intestine that comes in contact with food. Your small intestine is where most nutrient absorption happens. The inner wall of the intestine is lined with tiny finger-like projections called villi that absorb nutrients into your bloodstream.
When surgeons bypass a portion of your small intestine, they're essentially reducing the "absorption surface area." Imagine having a sponge to soak up water—if you make the sponge smaller, it absorbs less. Similarly, with less intestine available to absorb nutrients, your body takes in fewer calories from the food you consume.
Hormonal Changes
Something fascinating happens after these surgeries that scientists are still working to fully understand. When food bypasses certain portions of your digestive tract, it changes the production of gut hormones that control hunger, fullness, and even blood sugar.
For example, levels of a hormone called GLP-1 often increase after surgery. This hormone helps you feel full, slows stomach emptying, and improves insulin sensitivity. Other hormonal changes can reduce hunger and improve your body's metabolism.
These hormonal effects explain why many patients experience reduced hunger and improved diabetes even before significant weight loss occurs.
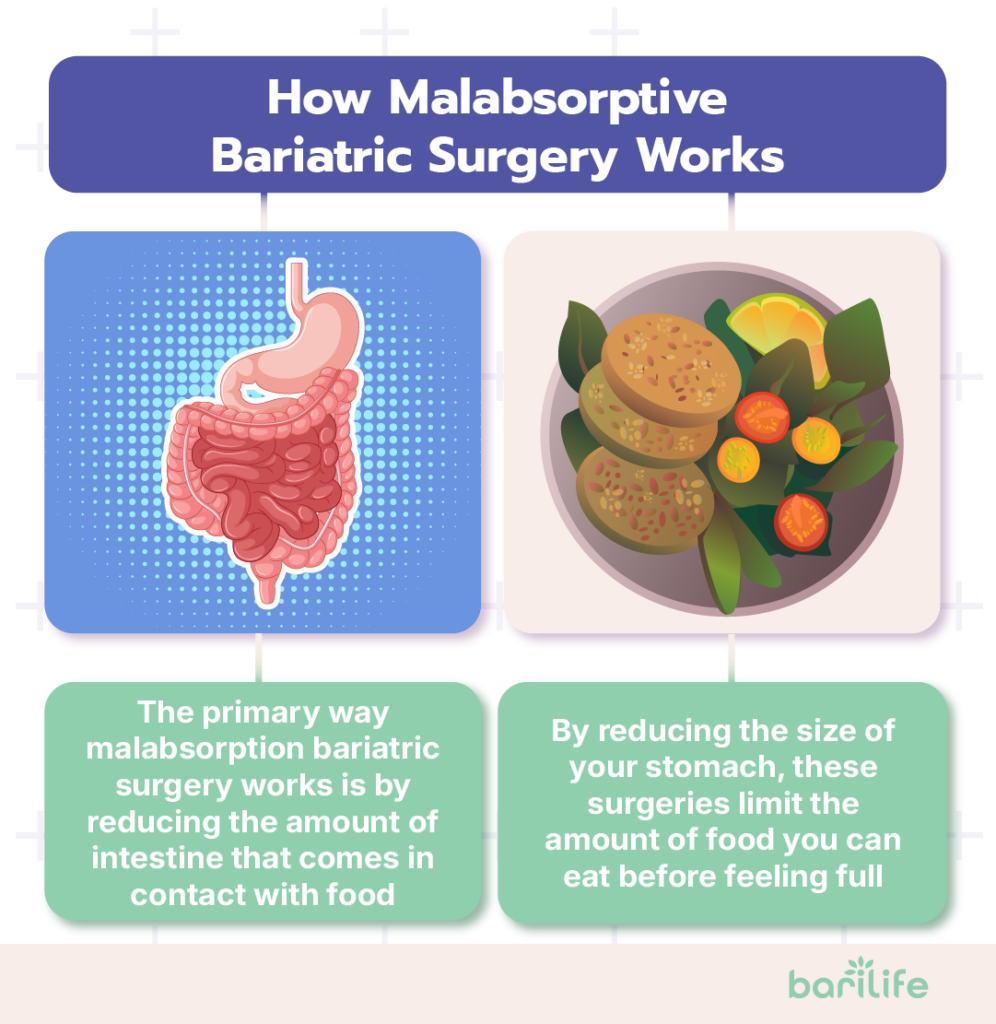
Restriction of Food Intake
While the primary mechanism is malabsorption, most of these procedures also include a restrictive component. By reducing the size of your stomach, these surgeries limit the amount of food you can eat before feeling full.
This combined approach creates a powerful weight loss effect that's difficult to achieve through non-surgical means.
Expected Outcomes of Malabsorptive Bariatric Surgery
What can you realistically expect if you choose one of these procedures? Here's what the research shows:
Significant Weight Loss
Malabsorptive procedures typically result in more dramatic weight loss than purely restrictive surgeries like the gastric sleeve or band.
This weight loss usually stabilizes around 18-24 months after surgery, though some patients may experience some weight regain over time. Still, most maintain significant long-term weight loss compared to their pre-surgery weight.
Improvement or Resolution of Comorbidities
One of the most remarkable benefits of these surgeries is their impact on obesity-related health conditions. Many patients see dramatic improvements in:
- Type 2 diabetes
- High blood pressure
- Sleep apnea
- High cholesterol
- Joint pain
- Fatty liver disease
Enhanced Quality of Life
Beyond the numbers on the scale or in your lab tests, these surgeries often lead to dramatic improvements in how you feel and what you can do.
Patients frequently report:
- Being able to move more easily and comfortably
- Having more energy throughout the day
- Feeling more confident in social situations
- Sleeping better
- Experiencing less depression and anxiety
- Being able to participate in activities they couldn't before
Benefits of Malabsorptive Procedures
What makes these particular surgeries stand out compared to other weight loss options? Here are the main advantages:
Effective Weight Loss
Simply put, restrictive and malabsorptive bariatric surgery procedures tend to produce more significant and durable weight loss than purely restrictive surgeries or non-surgical approaches. For people with severe obesity or who have failed other weight loss attempts, this can be life-saving.
Metabolic Improvements
One of the most fascinating aspects of malabsorptive procedures is their impact on metabolism, particularly in individuals with type 2 diabetes.
This "metabolic effect" appears to be related to changes in gut hormones and bile acid metabolism that happen when food bypasses portions of the gastrointestinal tract.
Long-Term Health Benefits
Research indicates that the health benefits of bariatric surgery lead to longer lives for many patients. Studies have found reduced rates of cardiovascular events (like heart attacks and strokes), certain cancers, and overall mortality in patients who undergo these procedures compared to similar patients who don't have surgery.
While all types of bariatric surgery can provide these benefits, the more substantial weight loss typically achieved with malabsorptive procedures may offer additional advantages for patients suffering from severe obesity or multiple health conditions.
Risks and Complications
Malabsorptive bariatric surgery can offer tremendous benefits, but it's important to understand the potential downsides as well:
Nutritional Deficiencies
This is perhaps the most significant concern with malabsorptive procedures. By design, these surgeries reduce your body's ability to absorb nutrients. While that's helpful for calories, it also means you'll absorb fewer essential vitamins, minerals, and proteins.
Common deficiencies include:
- Protein
- Iron
- Calcium
- Vitamin D
- Vitamin B12
- Fat-soluble vitamins (A, D, E, K)
To prevent these deficiencies, you'll need to take specific supplements every day for the rest of your life. You'll also need to get blood tests regularly to monitor your nutrient levels. This commitment is non-negotiable. Failing to take supplements can cause severe health problems like anemia, bone loss, or neurological issues.
Surgical Complications
As with any major surgery, there are risks during and shortly after the procedure, including:
- Bleeding
- Infection
- Blood clots
- Leaks at the surgical connections
- Bowel obstruction
However, complication rates have decreased significantly with improvements in surgical techniques and postoperative care.

Gastrointestinal Issues
Bariatric surgery malabsorption can cause some unpleasant digestive symptoms, especially if you don't follow dietary recommendations. These can include:
- Diarrhea
- Frequent, foul-smelling stools
- Gas and bloating
- Dumping syndrome
These symptoms can often be managed by making adjustments to your diet, but they represent a significant lifestyle consideration.
Lifestyle Adjustments and Long-Term Considerations
If you're considering malabsorptive bariatric surgery, it's essential to understand the lifelong commitments involved:
Dietary Changes
Your relationship with food will change dramatically after surgery. You'll need to:
- Eat smaller portions
- Focus on protein-rich foods first
- Avoid foods that are high in fat and sugar
- Eat slowly and chew thoroughly
- Separate eating and drinking
- Take vitamin and mineral supplements consistently
Regular Monitoring
Successful outcomes require a lifelong partnership with your healthcare team. You'll need:
- Regular check-ups (typically every 3-6 months the first year, then annually)
- Blood tests to monitor nutritional status
- Periodic adjustments to your supplement regimen
- Ongoing support for any complications that arise
Physical Activity
Exercise becomes both easier and more important after surgery. Regular physical activity helps:

Leave a Comment
Your email address will not be published.