Key Takeaways
- Bariatric surgery has evolved from early, rudimentary weight loss procedures to highly advanced, minimally invasive techniques that not only aid in weight loss but also improve metabolic health.
- The introduction of laparoscopic and robotic-assisted surgery has made bariatric procedures safer, with shorter recovery times and fewer complications, increasing accessibility for patients.
- Ongoing research in personalized medicine, gut hormone regulation, and metabolic surgery is shaping the future of bariatric care, offering more tailored and effective treatment options for obesity and related conditions.
The history of bariatric surgery is a fascinating journey through medical innovation.
The concept of surgical weight loss dates back to 10th-century Spain. History records a king, Sancho of Leon, who was so obese that he couldn’t walk, ride his horse, or even wield a sword. His weight would cost him his throne.
A renowned Jewish physician, Hasdai Ibn Shaprut, performed the first documented weight loss surgery. He sutured the king’s lips together and forced him to eat a liquid diet of herbal medicines. The primitive but effective procedure helped the king lose half his body weight and regain his throne.
The roots of modern bariatric surgery trace back to the 1950s when surgeons noticed that individuals who had parts of their stomach removed for ulcers or cancer experienced significant and sustained weight loss.
Surgeons at the time began challenging the conventional view that obesity was simply a willpower issue. They decided to treat obesity as a medical condition that may benefit from surgical intervention. Their willingness to explore this idea eventually opened up an entirely new field of medicine.
Read on to learn more about the fascinating history of bariatric surgery and understand how does bariatric surgery work.
Table of Contents
Early Surgical Techniques
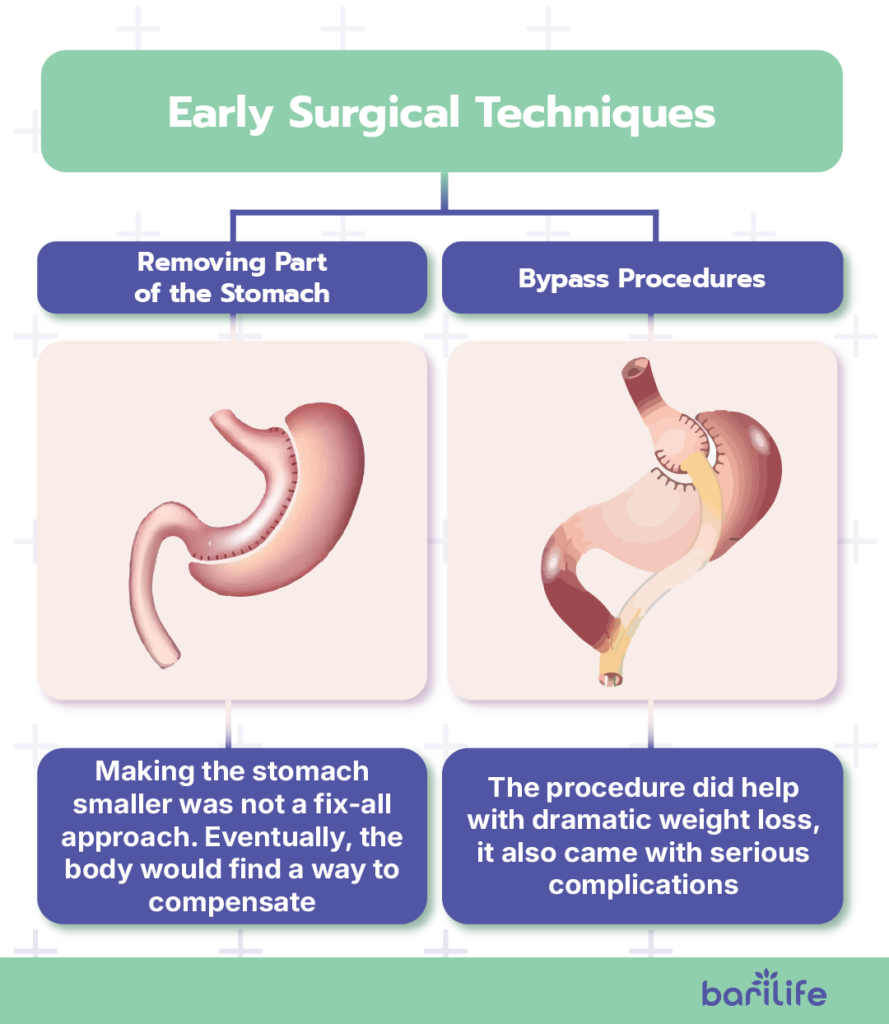
The earliest attempts at bariatric surgery were quite simple. Surgeons removed large portions of the stomach to limit a person’s food intake.
Removing Part of the Stomach
These initial procedures, while straightforward, represented the first surgical attempt to help patients with severe obesity. However, they discovered that the human body is remarkably adaptable. Some individuals found ways to eat around these restrictions, gradually stretching their reduced stomachs.
The surgeons learned an important lesson—making the stomach smaller was not a fix-all approach. Eventually, the body would find a way to compensate, often returning to its accustomed eating habits.
Patients who underwent these procedures soon found that maintaining proper nutrition required significant dietary changes, often supplemented with bariatric multivitamins, bariatric vitamins for hair loss, and bariatric calcium chews to prevent deficiencies.
Bypass Procedures
Later, in the 1960s, surgeons experimented with another approach. Instead of making the stomach smaller, they tried bypassing parts of the intestine where food is absorbed. This method is known as a malabsorptive procedure.
The thinking behind this method was different: instead of limiting the amount of food consumed, the procedure would limit the amount the digestive system could absorb.
This technique, known as the jejunoileal bypass, would become the first widely performed weight loss surgery.
While the procedure did help with dramatic weight loss, it also came with serious complications. Individuals developed nutritional deficiencies, liver problems, and other life-threatening issues.
Many people had to have the procedure reversed, and some suffered long term effects of bariatric surgery because of it. This period became known as the “learning years” in bariatric surgery.
As a result, patients who underwent these procedures often required bariatric vitamins, bariatric multivitamin with iron, and bariatric probiotic supplements to maintain essential nutrient levels.
Important Lessons
Although these failures and complications were undoubtedly disappointing, they also taught health professionals essential lessons about the complexity of the human body and maintaining proper nutrition.
These lessons would later help surgeons develop more sophisticated techniques that balanced weight loss with safety.
Surgeons also realized how important it is to qualify patients and to do long-term follow-up care after the procedure.
Significant Surgical Innovations
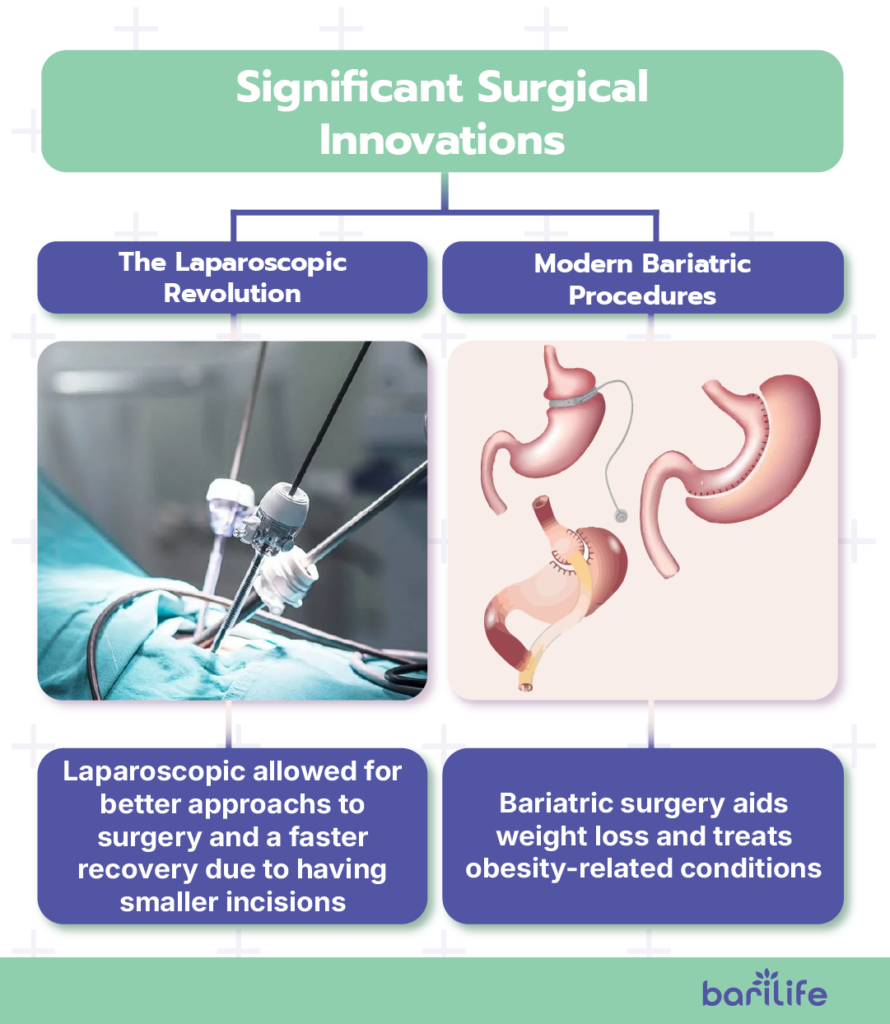
In the 1970s and 1980s, surgeons began developing hybrid procedures that combined moderate restriction (e.g., making the stomach smaller) with limited malabsorption (e.g., rerouting a portion of the intestine).
These procedures were much safer and more effective for weight loss. The most notable of these procedures was the roux-en-y gastric bypass, which became the gold standard for bariatric surgery for many years.
Surgeons could modify the degree of restriction and malabsorption based on the patient’s unique needs. This approach solved many problems that earlier procedures could not.
The Laparoscopic Revolution
The introduction of laparoscopic surgery in the 1990s dramatically changed the approach. Instead of making large incisions, surgeons could perform complex procedures through several incisions, each measuring only 0.25 to 0.5 inches.
High-definition cameras and specialized instruments inserted through the tiny incisions allow surgeons greater precision. The smaller incisions also mean less trauma and scarring, allowing people to recover faster.
Weight loss surgery has become much safer and more accessible than ever before. This advancement significantly improved the success rate of bariatric surgery.
Modern Bariatric Procedures
Today, we have newer procedures that look remarkably different from earlier operations. We now have modern techniques like sleeve gastrectomy and gastric bypass.
Bariatric surgeries not only help with weight loss but also resolve many obesity-related health issues like diabetes, sleep apnea, and high blood pressure.
Laparoscopic lap band surgery is also available. In this procedure, a surgeon places an adjustable band around the stomach to control how much food can be eaten. While the weight loss from this procedure is not as significant as that from some other bariatric surgeries, it is more easily reversible.
Research also reveals that bariatric surgery impacts the production of various gut hormones that influence hunger, satiety, and blood sugar control. These findings explain why people often experience improvements in their diabetes symptoms.
Additionally, some patients may wonder, “can you have bariatric surgery twice?” The answer depends on the individual case. Some people require a revision surgery due to complications, weight regain, or changes in medical status.
Obesity As a Public Health Issue

Obesity has become a significant global health crisis, with rates rising dramatically over the past several decades. According to the World Health Organization, one in eight people were living with obesity in 2022. Obesity has more than doubled since 1990.
It is now recognized as a major public health concern due to its strong association with serious health conditions, including type 2 diabetes, heart disease, high blood pressure, and certain cancers. The increasing prevalence of obesity has contributed to higher rates of morbidity and mortality, placing a growing burden on healthcare systems worldwide.
Governments and health organizations have taken steps to address the obesity epidemic through various policy initiatives.
Nutritional labeling requirements, public awareness campaigns, and programs promoting physical activity and healthy eating have been implemented to encourage healthier lifestyle choices. These initiatives aim to reduce the impact of obesity by helping individuals make informed decisions about their diet and overall health.
Despite these efforts, obesity remains a complex issue influenced by multiple factors, including genetics, environment, socioeconomic status, and behavioral habits.
Addressing obesity as a public health issue requires a multifaceted approach, including education, policy changes, and accessible treatment options, to improve outcomes for individuals and communities.
While health professionals continue to address the rising obesity rates, the focus has shifted more towards prevention, especially in younger people. It’s much more achievable to keep a healthy weight than to lose it later.
From Last Resort to Life-Changing
It used to be that bariatric surgery was only performed as a last resort for people with a BMI over 40.
However, when doctors noticed that bariatric surgery helps with certain conditions, especially diabetes, they started making it more available to individuals with lower BMIs, especially those with uncontrolled diabetes.
Today, some people might qualify for the surgery even if they have a BMI as low as 30 if they have severe metabolic concerns.
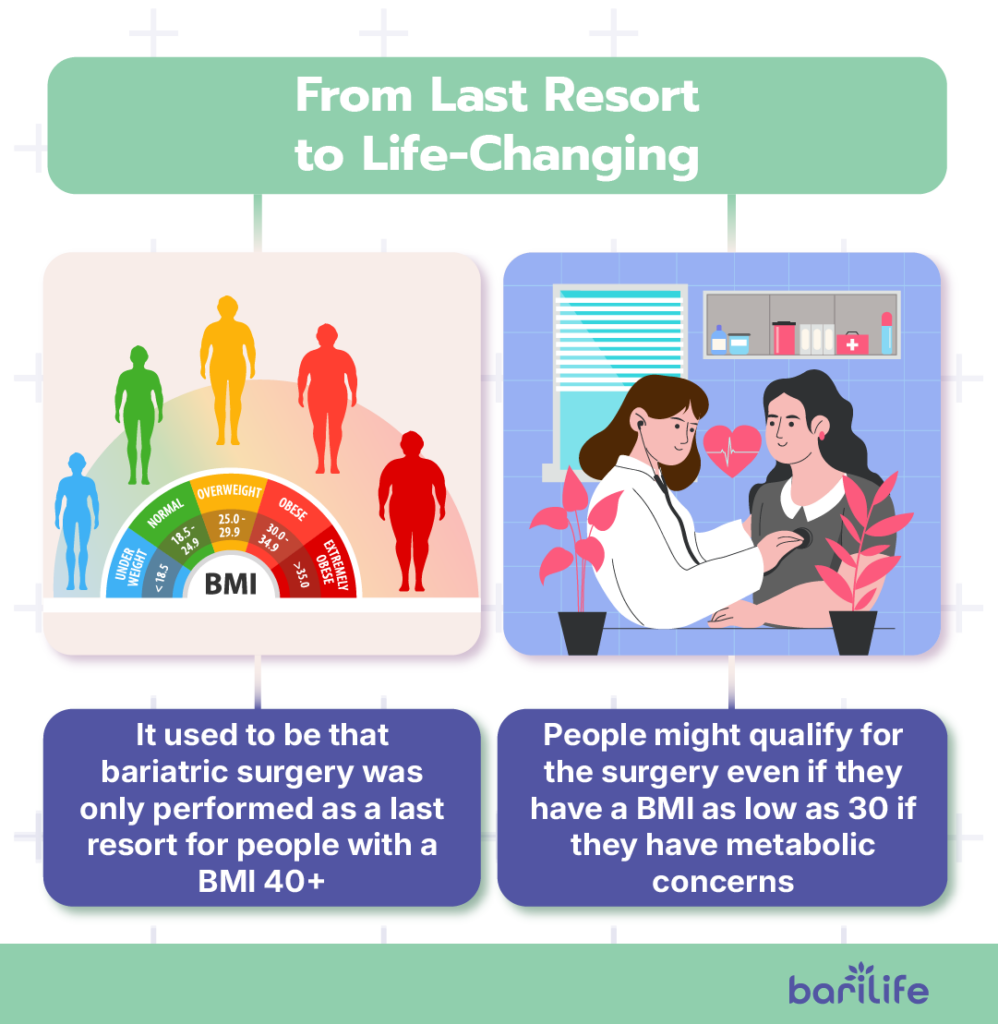
This change led to a new term: metabolic surgery. It demonstrates a newer understanding of how these procedures do more than just help with weight loss—they change how the body processes food and uses energy by altering gut hormones and even the beneficial bacteria in your digestive system.
Research continues to help us recognize who would benefit the most from these procedures. We’re also developing new techniques that are less invasive while still providing the metabolic benefits that make these surgeries so effective.
The Future of Bariatric Surgery
The future holds promising developments that could dramatically change how obesity is treated. Researchers are now focusing on even less invasive procedures while maximizing effectiveness.
Robot-assisted surgery is becoming more prevalent, giving more precision and control over procedures. We now also have 3D visualization, which helps improve maneuverability and can lead to better patient outcomes.
Personalized medicine is another thing we can look forward to. Genetic testing and metabolic profiling help surgeons identify which procedure would work best for each patient. Matching patients with the best surgical solution can greatly improve success rates and reduce complications.
Ultimately, the goal of today’s developments is to come up with more effective, safer, and personalized solutions for patients who struggle with obesity and its related conditions.
How Bari Life Can Help
Despite modern advancements in the development of bariatric surgery, nutritional deficiencies remain a common issue after surgery.
Proper nutrition is key to long-term success after bariatric surgery, and Bari Life supplements make it easy to get the essential vitamins and minerals your body needs.
Designed specifically for before and after bariatric surgery, these supplements help prevent deficiencies, support recovery, and keep you feeling your best.
Don’t let nutrient gaps hold you back—choose Bari Life for a healthier journey post-surgery!

Conclusion
The evolution of bariatric surgery is a testament to medical innovation, shifting from rudimentary weight loss techniques to highly sophisticated procedures that not only promote weight loss but also improve metabolic health. From the early days of stomach resections to modern laparoscopic and robotic-assisted surgeries, advancements have made these procedures safer, more effective, and more accessible.
As obesity remains a pressing public health concern, bariatric surgery has transitioned from a last-resort option to a life-changing treatment for individuals with metabolic disorders. The field continues to evolve, with research focusing on personalized medicine, gut hormone regulation, and minimally invasive techniques. Looking ahead, the integration of technology and a deeper understanding of metabolic health will further enhance bariatric care, offering more precise and patient-tailored solutions.
If you want to learn more, why not check out these articles below:
Resources
Faria, G. R. (2017). A brief history of bariatric surgery. Porto Biomedical Journal.



What are your tips and tricks to post-bariatric success?