ENTER YOUR EMAIL ADDRESS TO UNLOCK
15% OFF
on your first order
Some exclusions apply.
What we do know: First, let’s discuss what the current literature on this topic has discovered. As with vitamin supplementation research on bariatric patients, the studies on oral health after bariatric surgery are quite limited. Dr. Boyce’s research on 309 gastric bypass patients is the largest study on the topic of vitamin deficiencies and the efficacy of recommended supplementation after bariatric surgery.
In reviewing the current literature concerning dental manifestations after weight loss surgery we found that all of the literature noted increased dental erosion, increased dental caries (is a breakdown of teeth due to activities of bacteria), and increased dental hypersensitivity after weight loss surgery.
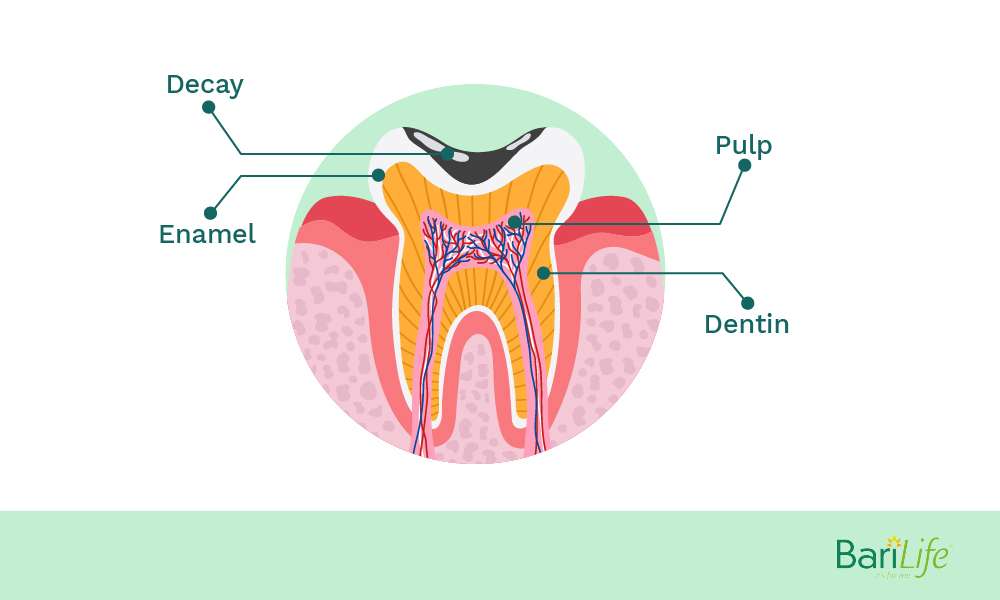
Dental erosion is defined as a chemical dissolution of dental tissues by a chemical process (acid or chelating agents) without bacterial involvement. The acid in the food and drink and gastric acids from vomiting and reflux can lead to the softening of the tooth enamel.
As the dental hard tissues soften, the area is more susceptible to break down from abrasion. The acidic attack is irreversible.
Most articles blame the increase of exposure to gastric juices because of vomiting and reflux as a reason for the increased erosion after bariatric surgery.
You were probably told by your dietitian to eat several small meals throughout the day to fend off hunger – and it does! However, this may be attributed to increasing a bariatric patient’s risk of developing dental caries by allowing more bacterial growth compared to eating the usual three meals a day.
Dental Hypersensitivity is reported by a large number of patients after weight loss surgery. One study published in Obesity Surgery found that the most common variable associated with visits to the dentist after surgery was dental hypersensitivity. Hypersensitivity represents a condition of a presumable complex pathology.
[box]
Two processes are essential for its development:
1. Dentin must be exposed through genetic disturbance, enamel defect, loss of enamel (erosion, abrasion, attrition, abfraction), gingival recession with rapid loss of cementum and
2. The dentin tubules must be open to both the oral cavity and the pulp. One interesting study followed 54 patients and found that 25 % of the patients had more tooth decay, erosion, and hypersensitivity than before bariatric surgery.
[/box]
Vitamin deficiencies can also play a part in tooth decay and erosion. Common deficiencies after bariatric surgery include protein, iron, calcium, vitamin D, vitamin B-12, vitamin A, vitamin K, zinc, magnesium, and vitamin C. These deficiencies can negatively impact the immune system and bone turnover rate as well as increase the risk of periodontal disease. Protein deficiency occurs in 13%-18% of patients after surgery.
The incidence of vitamin D deficiency may be as high as 63% in patients 1-4 years post-bariatric surgery. According to Dr. Boyce, 75-80% of his patients have vitamin D deficiencies PRIOR to surgery. Vitamin B-12 deficiency is associated with the risk of osteoporosis and anemia. Vitamin C is frequently deficient among this patient population and can lead to gingivitis and increased gingival inflammation.
So most of the research published about the link between increased tooth decay and bariatric surgery points to vomiting, gastric reflux, reduced saliva, more acidic saliva, vitamin deficiencies, and frequent meals.
How do we explain the increased tooth decay of those patients who insist they take their vitamins and have no deficiencies and also do not report excessive vomiting and reflux? There are many patients who fall into this category.
Check out the many patient comments found on Bariatric Surgery Source’s website: Dental Problems After Gastric Bypass Surgery
Our question is, “What kind/form of vitamins are these patients taking?” Most bariatric patients have been instructed to take chewable vitamins after surgery because many of the popular bariatric brands promote chewable vitamins.
At the New Life Center for Bariatric Surgery, patients are instructed to use Bari Life’s dissolvable complete bariatric vitamin powder after surgery, and many switch to the Bari Life complete bariatric vitamin tablet after 4-6 weeks. As you will recall, The New Life Center for Bariatric surgery reports very few cases of tooth decay in patients after surgery.
Could chewable vitamins be the culprit or compounding the problem?
Dentists will tell you to avoid gummy vitamins and suggest that chewable vitamins can cause problems for your teeth. One little known disadvantage of chewable supplements is that they may damage tooth enamel. There is some evidence that chewable vitamin C tablets can stain teeth.
The dosage for most bariatric chewable vitamins can be as many as 8-10 large chewable tablets per day. Patients will literally chew their vitamins all day long. Chewable vitamins get stuck in between the teeth and will remain there for long periods of time. According to one article, foods that contain the four fat-soluble vitamins, A, D, E, K as well as vitamin C is good for your teeth if you do not chew the supplements directly.
Malabsorption of calcium after bariatric surgery Bariatric surgery affects absorption within the gastrointestinal tract. To get all the required vitamins and minerals after surgery, supplementation is essential. While you may not notice deficiencies in certain vitamins or minerals right away, long term consequences exist. If not addressed, negative health outcomes can occur.
Malabsorption occurs after bariatric surgery because of an alteration in the gastrointestinal tract. These alterations can be either restrictive or malabsorptive in nature. In restrictive bariatric procedures, gastric volume decreases due to a change in stomach size. With malabsorptive procedures , the stomach is bypassed. Because of the change in the anatomy of the GI tract in all bariatric surgery, absorption changes.
Bariatric procedures affect absorption through a reduction in stomach volume, a change in intestinal surface area , gastric pH changes, and an alteration in the speed of gastric emptying. These changes affect how the body is able to absorb nutrients from food.
One mineral that is essential to supplement after bariatric surgery is calcium. In a study completed on post-gastric bypass patients, calcium absorption decreased significantly after surgery, dropping from over 30% to less than 10% after surgery .
Along with a substantial drop in calcium absorption, malabsorption begins soon after surgery. Calcium malabsorption is documented as early as 3 months after bariatric surgery , providing significant evidence to begin supplementation early.
What happens if I don’t get enough calcium? Calcium plays an important role in the body. It supports your skeletal structure and your teeth, providing structure, hardness, and support in maintaining and creating healthy bones and teeth. Calcium is so important that it even plays a further role in dental health, protecting your gums against irritation and gum disease .
It’s fair to say that if you aren’t getting enough calcium, there can be significant consequences, both short term and long term. If you aren’t getting enough calcium after surgery , your body starts taking it from various calcium deposits in your body. These deposits primarily exist in your bones and teeth. If enough calcium is taken from these deposits it can lead to weak bones, osteoporosis, and brittle teeth.
More specifically, when calcium is taken from your teeth, dental health issues occur. This creates a higher risk of tooth damage, tooth decay, and brittle teeth. If supplementation is not prioritized, these issues can become worse and create substantial problems.
The great news is, supplementing with calcium after surgery is an easy way to support your bones and teeth. By taking a calcium supplement, you protect your bones and teeth from complications that can occur because of low calcium.
Calcium requirements for bariatric patients Getting enough calcium after bariatric surgery can be difficult. To be best absorbed, calcium needs the right gastric pH. This puts post-bariatric surgery patients at higher risk for deficiency because of a decrease in gastric pH after surgery. Because of this, calcium supplementation is required to meet daily nutrient requirements.
There are two different forms of calcium available for supplementation: calcium citrate and calcium carbonate. Because calcium carbonate is not as easily absorbed, calcium citrate is preferred. Here’s why.
After bariatric surgery, stomach acid is reduced. Less stomach acid is required for the absorption of calcium citrate, making it ideal for bariatric patients. It also causes less stomach upset and does not need to be taken with food .
While calcium is obtained from foods like dairy products, green leafy vegetables, and fish with bones, it is nearly impossible to get the recommended daily amount through food alone after bariatric surgery. With supplementation, calcium deficiencies are easy to prevent.
According to the ASMBS, 1,500 mg/day is ideal for post-bariatric surgery patients.
Bari Life has a great tasting Calcium chew to support calcium absorption after surgery. Three individual chews have 1,500mg of calcium citrate and 3,000 IUs of Vitamin D3 to support absorption. It is a complete calcium supplement to support your health after bariatric surgery.
Curiouser and curiouser… The information provided by the medical community concerning the correlation of tooth decay and bariatric surgery does not mention chewable vitamins, only vitamin deficiencies as a possible cause. One article states that the medical literature has inadequately reported the potentially deleterious effects of such surgery on dental health.
The dental professional community makes it very clear that vitamin and mineral supplementation in the form of gummies, soft chews, or tablet chewable vitamins can cause problems that can lead to tooth decay and very poor dental health.
It makes sense that when all of these conditions come together, vomiting, reflux, acidic saliva along with food and vitamins sitting for hours in-between teeth and other bariatric surgery complications, there becomes an increased risk for tooth decay. There is no research available discussing the effects of chewable vitamins and tooth decay after weight loss surgery. If you are experiencing excessive tooth decay and have had bariatric surgery you should seek professional medical and dental consultations.
It is extremely important to have your lab work completed at least annually to look for vitamin and mineral deficiencies and have your dentist advise you on the special care for your teeth. You may need to eat less sticky, less acidic foods, and avoid chewable vitamins.
You may need to brush and floss more frequently and have regular fluoride treatments to counteract the acidic saliva. It’s actually been proven in studies that elderly people with better oral health are more resistant to all-cause mortality (death from all causes). What’s more – studies prove that people with chronic periodontal disease and exposure to oral bacteria are at greater risk of developing heart disease!
The Bottom Line: Clearly, the dental health of patients after bariatric surgery is something that needs more research in order to determine and treat the cause of increased tooth decay after surgery.
It should be noted that proper dental hygiene is key in not only maintaining strong and healthy teeth after surgery but also lower your risk of all-cause mortality and heart disease.
Take care of your teeth, every day!