What you need to know about requirements before gastric sleeve resection surgery
Bariatric surgery is an effective treatment for obesity that assists with weight loss and improves metabolic comorbidities, such as diabetes, hypertension, sleep apnea, arthritis, and metabolic syndrome. The preoperative evaluation is crucial to ensure the best outcome possible. Your healthcare team’s assessment and preparation for bariatric surgery improves your care and increases your chances for favorable results.
Overview of gastric sleeve
Laparoscopic gastric sleeve surgery is one of the types of weight-loss surgery. This procedure is done through very small incisions in your abdomen. Your surgeon will be removing a long section of your stomach to decrease the amount of food you can eat and decrease your appetite. About 80% of the stomach is removed. The procedure also causes hormonal changes in the body that reduce your appetite.
There isn’t any bypass of your bowel in this procedure. It is not reversible, but it is a safer procedure than other bariatric surgery types, with fewer complications after surgery. It is also sometimes used to help you lose enough weight so that another type of surgery can be done, like a gastric bypass.
Pre-surgery requirements
Currently, institutional guidelines and insurance requirements vary, but according to the SAGES (Society of American Gastrointestinal and Endoscopic Surgeons) guidelines for bariatric surgery, the indications for weight loss surgery are as follows:
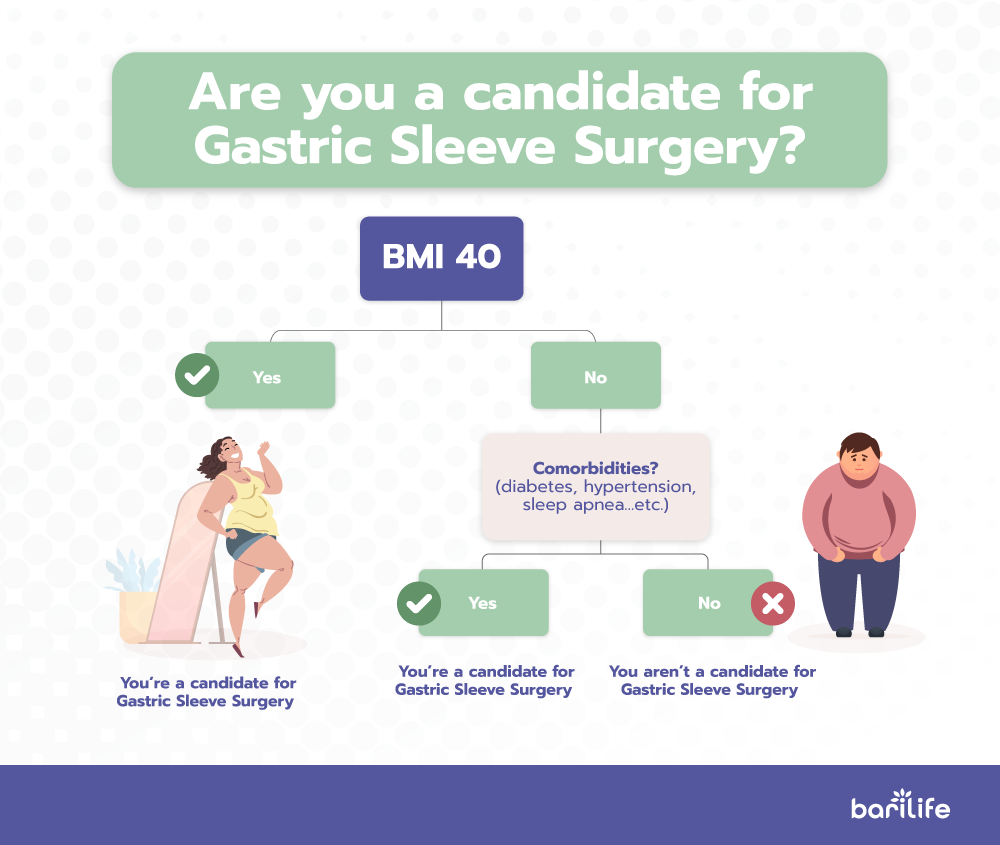
- BMI more than 40 without comorbidities
- BMI 35 to 39.9 with at least one serious comorbidity, including:
- Diabetes
- Hypertension
- Sleep apnea
- Limitations in the quality of life
It is important to know that once you are in a bariatric surgery program and before surgery, you may be required to participate in a guided weight loss program with exercise and lifestyle modifications. This helps ensure that you can make the commitment necessary to adhere to the postoperative nutritional restrictions of the procedure, and it also helps shrink the liver for safer surgery.
Reasons to not have gastric sleeve surgery
There are several reasons to not have bariatric surgery procedures, which include:
- Major depression or an uncontrolled mental health problem
- Current substance misuse, including alcoholism
- Patients determined to be non-compliant with nutritional requirements and supplementation after surgery
- Underlying eating disorders
- Severe coagulopathies
- Health-related contraindications (cardiovascular risk, anesthetic risk)
A problem with the sleeve gastrectomy is gastroesophageal reflux disease (GERD), which can worsen after a sleeve gastrectomy.
Pre-op evaluation
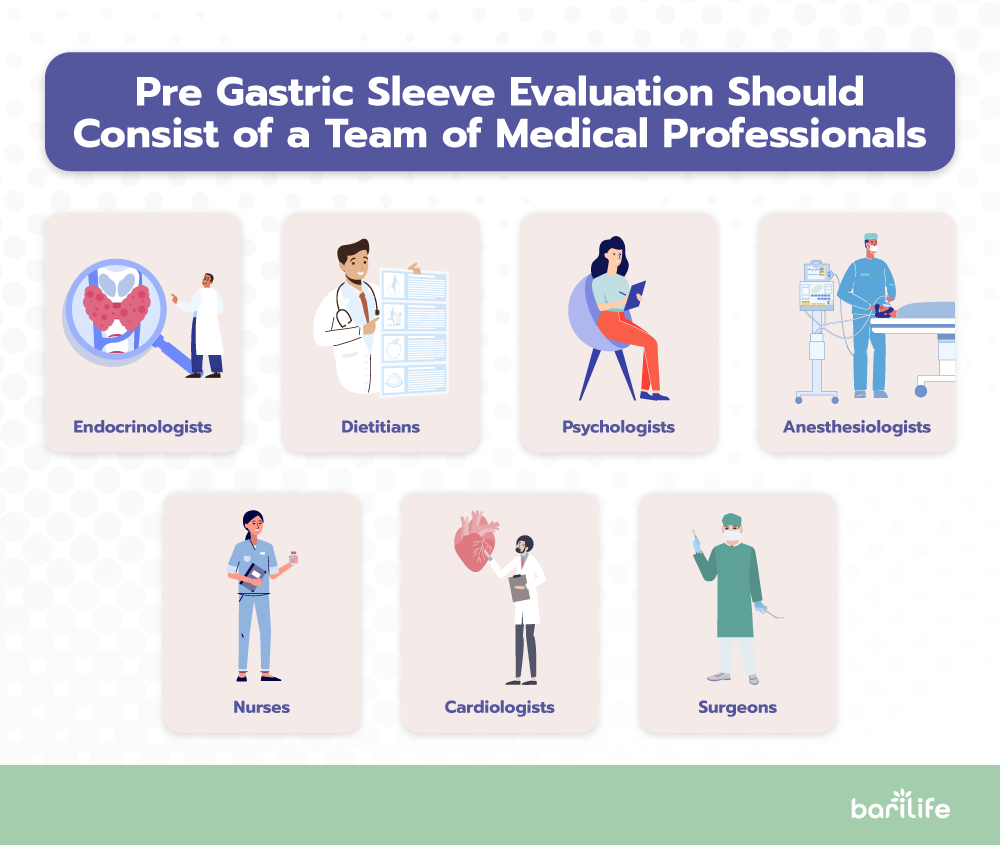
Your preoperative evaluation should include an assessment by a professional team that includes endocrinologists, dieticians, psychologists, anesthesiologists, nurses, cardiologists, and the surgeon.
Psychological evaluation
You should be psychologically fit to undergo bariatric surgery. A psychological clearance is one of the first steps in your preoperative workup. You will most likely undergo evaluations for a history of mental disorders, depression, eating disorders, prior weight loss attempts, compliance with therapy, and substance misuse.
If you have alcohol dependence, you need a referral for rehabilitation and detoxification before the procedure. You should have at least one year of abstinence before surgery.
Smoking cessation will be encouraged and documented before proceeding with the operation; quitting smoking improves outcomes and reduces postoperative complications. Some surgeons will require a blood test to verify the absence of nicotine before your surgery.
Your support system should also be evaluated. Studies have shown that patients with strong family and community support are more likely to have better outcomes.
Nutritional evaluation
A nutritional assessment and patient education will help guide you towards the necessary dietary modifications after surgery. Education regarding your expectations should also be included to ensure clear objectives regarding weight loss.
As a general rule, when having a sleeve gastrectomy, you should expect to lose about 60 to 65 percent of your excess body weight over two years. Weight maintenance strategies should be a topic of discussion with your doctor.
If you have diabetes and bariatric surgery, glycemic control is critical. A licensed dietician typically performs your nutritional evaluation.
Weight loss plan
A guided weight loss plan will be necessary, as a documented weight loss program can improve outcomes after your surgery. Your progress should be monitored during every office visit before your surgery.
Failure to lose weight due to lack of adherence to the plan and diet can predict how reliable you will be with lifestyle modifications needed after surgery. Even while following the plan, the inability to lose weight should be documented so that more intensive support can be provided before and after your surgery.
Medical clearance
A complete evaluation is necessary before you’re cleared to undergo surgery. This evaluation should include a detailed history and physical, a review of your past medical and surgical history, a review of psycho-social factors that could influence weight loss (employment, housing, family), a laboratory workup, and body measurements.
You should also complete cardiac disease and obstructive sleep apnea (OSA) screening. Your doctor should refer you for a sleep study if you have sleep apnea symptoms.
Your laboratory workup should include a comprehensive metabolic panel (CMP), complete blood count (CBC), levels of iron, vitamins, folate, type and screen, hemoglobin, and a coagulation panel.
Preoperative imaging
There are no guidelines regarding imaging before gastric sleeve surgery. If you have had previous bariatric surgery or any type of surgery that may have changed the anatomy of the gastrointestinal (GI) tract, your doctor may order imaging tests. Imaging can help your surgeon determine what type of bariatric surgery is best for you.
Other considerations
Esophagogastroduodenoscopy (EGD) is not routinely recommended in the workup for bariatric surgery. The American Society of Metabolic and Bariatric Surgery (ASMBS) advises only using endoscopy for patients with significant gastrointestinal (GI) symptoms.
Anesthetic considerations
Anesthesia evaluations are critical because obesity can cause health problems that make surgery difficult and cause problems after surgery. The obesity-related conditions include:
- Heart disease
- Hypertension
- Stroke
- Type 2 diabetes
- Gastroesophageal reflux disease
Evaluation of cardiorespiratory status
You should be evaluated for:
- Ischemic heart disease
- Systemic and pulmonary hypertension
- Right or left ventricular failure signs
- Sleep-disordered breathing
In addition to the standard ECG, further cardiac evaluation may include stress ECG (echocardiography) and cardiopulmonary exercise testing.
Insurance requirements
Bariatric surgery insurance coverage varies by insurance company. If your policy covers weight loss surgery and you meet the qualification requirements, most companies will pay for gastric sleeve surgery.
Most plans require you to pay part of the costs, such as copays, deductibles, and coinsurance.
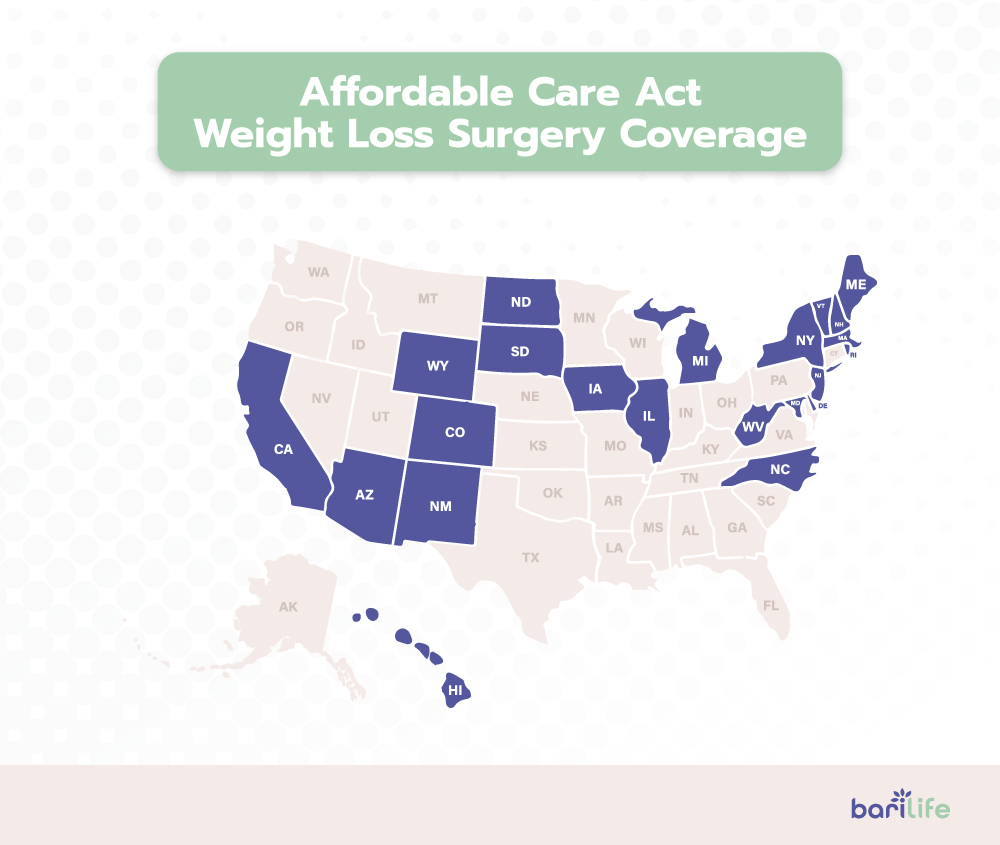
Affordable Care Act coverage
With the Affordable Care Act, insurance companies in 23 states are required to cover weight loss surgery for all Individual Plans, Family Plans, and Small Group Plans (employers with fewer than 50 full-time employees). The list below includes all Affordable Care Act states that cover weight loss surgery:
- Arizona
- California
- Colorado
- Delaware
- Hawaii
- Illinois
- Iowa
- Maine
- Maryland
- Massachusetts
- Michigan
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Rhode Island
- South Dakota
- Vermont
- West Virginia
- Wyoming
To confirm your coverage, you have a couple of options:
- Option 1 (recommended): Your local surgeon will contact your insurance company to confirm your benefits at no cost to you (even if you don’t move forward with surgery). Their office will be very familiar with your insurance company’s requirements and approval process, so it’s usually good to let them do the work for you.
- Option 2: Contact your insurance company yourself and check your Summary Plan Description (SPD). See this page on Insurance That Covers Bariatric Surgery for the complete list of United States insurance companies, contact information, and bariatric surgery coverage requirements.
Medicare and Medicaid
Medicare and Medicaid both cover bariatric surgery as long as you meet the qualification guidelines:
- A body mass index (BMI) over 35
- At least one comorbidity (health problem) related to obesity
- You must have documentation in your medical records confirming that previous attempts with medical treatment weight loss have been unsuccessful
If you meet each of the above criteria, Medicare and Medicaid will cover the following procedures:
- Gastric sleeve surgery (laparoscopic only)
- Gastric bypass surgery (open or laparoscopic)
- Lap band surgery (laparoscopic only)
- Biliopancreatic diversion with duodenal switch (BPD/DS) (open or laparoscopic)
You will need a referral from your primary care physician to a bariatric surgeon to be approved. Your surgeon will also need to be listed in The Centers for Medicare and Medicaid Services (CMS) directory.
If your plan includes bariatric surgery insurance, you will need to meet all of your insurance company’s coverage criteria (click here for a list of insurance companies) to confirm your surgery’s “medical necessity.”
Assuming you follow all the guidelines and provide complete, accurate information requested by your insurance company, the process from start to finish can take anywhere from one month to one year. To prove to your insurance company that your surgery is medically necessary, the typical requirements are:
- Minimum body mass index (BMI) requirements to be confirmed by your physician:
- BMI over 40 or
- BMI over 35 with one or more of the following:
- Clinically significant obstructive sleep apnea
- Coronary heart disease
- Medically refractory hypertension
- Type 2 diabetes mellitus
- Complete a medically supervised diet program. Bariatric surgery insurance criteria for the length of the program range from 3 to 7 consecutive months.
- Schedule a consultation with your bariatric surgeon.
- Schedule a consultation with your primary care physician to obtain a medical clearance letter.
- Schedule a psychiatric evaluation to obtain a mental health clearance letter.
- Schedule a nutritional evaluation from a Registered Dietitian.
- Send all of the above documentation to your insurance company along with a detailed history of your obesity-related health problems, difficulties, and treatment attempts. The review process typically happens in under one month.
- The insurance company sends an approval or denial letter:
- If approved, your surgeon’s bariatric coordinator will contact you for scheduling.
- If denied, you can choose to appeal the denial.
Your surgeon’s office will be very experienced in managing the above process. It may have all of the required personnel on staff (registered dietitian, psychiatrist, bariatric coordinator) to help you meet all of the requirements.
If you get your insurance through your work and your employer has 51 or more full-time employees, it is entirely up to your employer to decide whether or not to cover weight loss surgery.
Post-surgery requirements
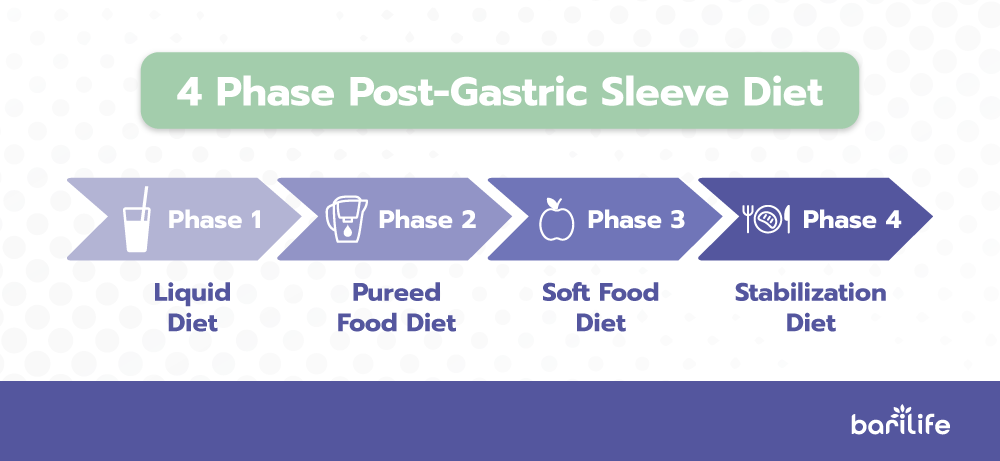
After sleeve gastrectomy surgery, your diet begins with sugar-free, noncarbonated liquids for the first seven days, progresses to pureed foods for three weeks, and finally to regular foods approximately four weeks after your surgery.
You will be required to take vitamin and mineral supplements for the rest of your life to prevent harmful deficiencies from forming.
You’ll have frequent medical checkups to monitor your health in the first several months after weight-loss surgery. You may need laboratory testing and other exams.
Post-surgery general guidelines
- Use an incentive spirometry bottle four times daily for ten days.
- You may walk, go up and downstairs and drive a car as soon as you feel up to it.
- Don’t lift more than 10 pounds the first three weeks.
- No activity restrictions after three weeks.
- Increased gas is expected in the first 3-6 weeks. You can try Gas-X or Di-Gel for relief.
- Take only the pain-relieving medications your surgeon advises you to take.
- Don’t take any anti-inflammatory pain medications unless approved by your surgeon, like Ibuprofen, Advil, Motrin, Naprosyn, Aleve, Daypro, Celebrex, Vioxx, and Bextra.
Take vitamin-calcium supplements daily post-bariatric surgery:
- Bari Life Just One Chewable with iron daily -OR- Bari Life Complete Bariatric Vitamin Formula Powder with calcium & iron.
- Calcium 1500mg plus Vit. D3 800 units (chewable for the first six weeks). Bari Life BariBurst Calcium Citrate Soft Chews.
- Bari Life’s Bariatric Balance – Diverse probiotics supplement to restore “good” bacteria to the gut
Female patients should not become pregnant until 18 months after surgery when weight loss has stabilized, or injury could occur to the unborn child. Female patients with menstrual periods should take chewable iron tablets daily until they reach menopause.
First post-op month diet
Dietary restrictions may vary by physician, but most use the following requirements.
Some drinks may irritate your healing stomach and should be avoided after surgery:
- No caffeine for at least three months after surgery
- No carbonated beverages for at least three months after surgery
- No alcoholic drinks for at least six months after surgery
Food intolerances
You may not be able to handle eating some foods after surgery:
- Red meat that’s tough or dry
- Greasy, high-fat foods
- Heavily seasoned or spicy foods
- Sugar alcohols, such as erythritol, glycerol, mannitol, sorbitol, and xylitol
- Foods reheated in the microwave
Week one
For the first week after the procedure, you will continue with the clear liquid diet you used in the days leading up to surgery. Doing so helps avoid postoperative complications like bowel obstruction, gastric leakage, diarrhea, constipation, and dehydration.
Week two
You will graduate to a full liquid diet during the second week after surgery. Options include:
- Instant breakfast drinks
- Unsweetened milk
- Protein powder shakes
- Sugar-free, nonfat frozen yogurt, ice cream, sorbet
- Sugar-free, nonfat pudding
- Thinned, hot cereal, such as Cream of Wheat, or oatmeal
- Fruit juices with no pulp, diluted with water
- Nonfat plain Greek yogurt
- Broth and cream-based soups without chunks, soft noodles are ok in very small amounts
- Protein soups and broths
During this period, you may feel an increase in your appetite. That is perfectly natural, but do not eat solid food. Your system is still not able to handle solid foods. Vomiting and worse complications can result. Fill up with liquids, and avoid sugar and fat to prepare yourself for the next stage. You should still avoid carbonated beverages and caffeine.
Week three
Now you can add soft, pureed foods to your diet during week three. Make sure to eat slowly and chew your food thoroughly, a minimum of 25 times, if you can. Any low-fat, sugar-free foods that you can puree, including lean protein sources and non-fibrous vegetables, is allowed. It’s important to begin increasing your protein intake. You can use pureed lean protein sources, no-sugar protein shakes, or eat eggs daily.
Week four
Now that you have made it to one-month post-surgery, you can begin adding solid foods to your diet. This is when you can put your new healthy-eating skills into action. Sugar, fat, and high-fat dairy, hard-to-digest foods such as steak, fibrous vegetables, pasta, white potatoes and nuts should all still be avoided. Beverages with caffeine can usually be reintroduced, in moderation, at this time.
Life-long diet restrictions
The goals of bariatric operations include maximizing weight loss and maintaining or achieving nutritional health while preventing micronutrient deficiencies and lean body mass loss.
Even though there are diet restrictions, there are plenty of things you are encouraged to eat after bariatric surgery.
Eat high protein foods first to get 60-80 grams of protein daily. Adequate protein intake prevents muscle and hair loss after surgery.
After protein, include non-starchy vegetables, including broccoli, cauliflower, and spinach. Next, add fruits or starchy foods. Starches like rice, pasta, and fried potatoes might make you feel bloated and gassy.
Eating three small meals a day, separating the food and fluids by thirty minutes, and chewing your food well will support your weight loss.
Now that you are eating solid food safely, focus on lean protein and vegetables. Introduce one food at a time so you can observe your body’s reaction. All foods can be included in your diet unless they trigger symptoms. Foods you should avoid entirely or only eat very occasionally are sugary sweets and soda.
Select nutrient-dense options, and avoid empty calories. Eating three small meals a day with minimal snacking might help you stick to your plan. Be sure to remain hydrated.
Vitamin and mineral requirements
Established guidelines recommend routine nutrient supplementation to include multivitamins, iron, minerals, calcium, and vitamin D. Deficiencies of micronutrients following bariatric surgery can arise from several mechanisms that include:
- Preoperative deficiency
- Reduced dietary intake
- Malabsorption
- Inadequate supplementation

Since obesity is already a risk factor for malnutrition and micronutrient deficiencies, all patients should be screened for deficiencies and correct them before surgery. The sleeve gastrectomy does not involve intestinal bypass, but it can still lead to nutritional deficits. Any bariatric procedure can result in malnutrition if proper nutrition management is not followed.
Bariatric surgery reduces the amount of nutrients your body receives, even when you are following a healthy diet. You will need to take vitamin and mineral supplements every day for the rest of your life. Start taking supplements when you begin the blended food stage of your diet.
The long-term health complications of weight-loss surgery can include:
- Neurological complications from a lack of B12
- Anemia due to a deficiency of iron or B12
- Your body absorbs calcium and vitamin D
- Bone and kidney disease due to changes in the way
The following vitamins and minerals are recommended:
Multivitamins
Vitamins need to be chewable or liquids for the first several 4-6 weeks after surgery. Choose a complete chewable multivitamin with iron, like Bari Life’s Just One Chewable. Avoid gummy vitamins and vitamin skin patches.
If you use an over-the-counter multivitamin, take one serving in the morning and one serving at bedtime. There are several multivitamins designed for people who have had weight-loss surgery.
Calcium
Daily calcium needs are 1,200 –1,500 milligrams (mg) per day after a sleeve gastrectomy or Roux-en-Y gastric bypass. The calcium in your food counts toward your daily goal. If your diet is high in calcium, adjust how much you take in supplemental form.
Your body can only absorb 500–600 milligrams of calcium at one time. To enhance absorption, take your supplement in three divided doses throughout the day. Take it with meals. Calcium citrate is the preferred form of calcium.
Vitamin D3
You will need 3,000 international units (75 micrograms) of vitamin D3 daily. Add up the amount of vitamin D in your multivitamin and calcium supplements to determine if you meet your vitamin D needs. If not, you may need to take an additional vitamin D3 supplement.
Bari Life’s solutions will give you 6,000 IU of Vitamin D3 – the amount clinically recommended by Dr. Boyce and has been used in his practice for 20+ years.
Vitamin B12
This supplement can be taken either by putting it under your tongue (sublingual) or an injection. If you are taking B12 orally, take 500 micrograms daily. If you choose to take B12 by monthly injection, you will need a prescription from your provider.
It is essential to review your vitamin and mineral levels annually. Your bariatric team should complete this review. Ensure your primary care provider knows you had weight loss surgery and checks your nutrient levels with an annual blood draw if that is not an option.
Conclusion
Here are a couple of things that you can do to prepare yourself for the best possible outcome after surgery:
Attend any seminars available in your area to learn as much as you can about your surgery and your life-long diet restrictions after surgery. Bariatric surgeons frequently hold seminars to educate potential patients and answer questions about bariatric surgery.
Speak with your surgeon and insurance company to find out the exact requirements for bariatric surgery. Your bariatric surgeon’s office will often take care of this step for you. They are very familiar with working with insurance companies and have staff dedicated to helping you get approved and meet the requirements for bariatric surgery.



What are your tips and tricks to post-bariatric success?