If you are planning to have the gastric sleeve procedure or have recently had the gastric sleeve procedure, then check out this article for a quick overview of recovery. This article will give you an overview of the recovery process and give you some tips on what to do in the first couple of months following surgery to enhance your recovery.
One of the most important parts of a good recovery is preparation and education. Make sure to meet with your surgeon and team of bariatric health professionals prior to surgery to go over what this process will look like for you. One reason this is important is that not everyone’s recovery will look the exact same.
Your team of bariatric health professionals will be able to further educate you on what you should expect and if there are any modifications that you might need to make to the standard recovery process.
It is also very important to note that most of your recovery process will likely take place in your home. So, it is important to prepare your home to suit your needs during recovery. One way to do this is to ask yourself questions like; do I have stairs in your house? Do I need to go up the stairs to go to bed? And can I easily access your bathroom?

Asking yourself questions like these in advance will help you identify any potential barriers to recovery that might be in your home. Once any potential barriers are identified, work to develop a plan to help you have the most comfortable recovery at home possible.
Don’t hesitate to ask your bariatric team any questions that you might have as you prepare for surgery.
The journey to recovery!
Before we get into a weekly outline of recovery, here are some quick tips for recovery from the gastric sleeve!
- Schedule and attend both pre-and post-op appointments
- Prepare your home or recovery space prior to surgery
- Walk around early and as often as you can
- Consume lots of fluids between meals not during mealtimes or within one hour following meals
- Follow each phase of the 4-phase diet
- Don’t be afraid to ask for support from a therapist or support group

The first few weeks following surgery can be a mix of emotions. On one hand you will likely feel relieved to know that you made it through surgery safely and excited to start the journey. On the other hand the aches and pains become reality and the road to recovery might feel like a large mountain to climb. Just know that it’s totally normal to have mixed emotions during your recovery process.
Recovery can be exhausting and challenging. It is important that you do not let negative feelings get in the way of your recovery. Be sure to take a step back, look at the big picture, and celebrate the small victories throughout your entire recovery process.
A timeline for recovery
Week 1
The first week of your bariatric journey is a very important step in your recovery process and setting good habits early can help promote long-term success.
Hospital stay
There are many enhanced recovery practices that can help you to optimize your recovery and a lot of them will likely be implemented during your hospital stay. They include:
- Walking and moving around with guidance from a physical therapist
- Drinking a full liquid diet
- Pain management
- IV fluids for hydration alongside oral fluid intake
- An extra session with a dietitian prior to discharge from the hospital

To be discharged from the hospital you must be free from complications, not require IV medications or fluids, and be able to tolerate oral diet and fluid intake.
Diet
Key points of the Liquid protein diet:
- Consume 64 oz per day
- Get adequate protein.
- Begin powder multivitamins
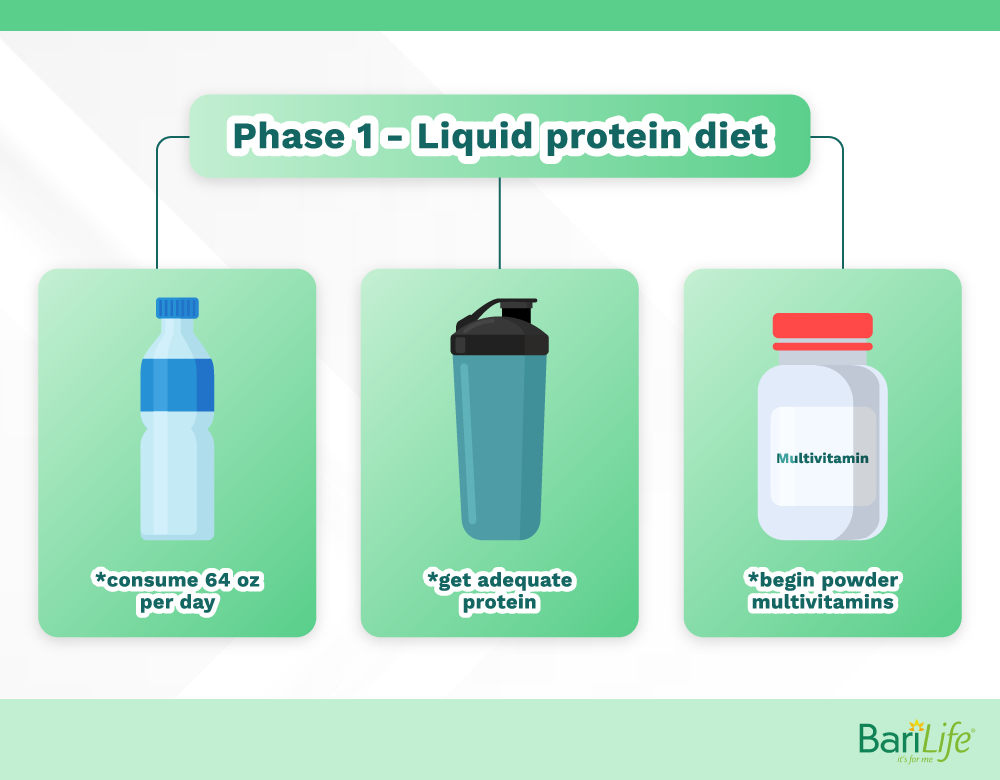
Make sure to consume a variety of liquids for nutrient density and electrolyte balance. Consuming excessive amounts of only water can cause electrolyte imbalances so be sure to incorporate some fluids containing electrolytes into your liquid diet.
Protein intake can be challenging when you are in the first few phases of the 4-phase diet. Incorporating protein supplements at each stage can help you to reach your protein goals. In general, women should try to consume 60g of protein or more and men should try to consume about 75g or more.
Wound healing
Your surgical incisions will still be tender and sensitive. It is important to take good care of your surgical incisions to prevent infection and promote healing.
Wash incisions with soap and water gently. Do not scrub or soak. Pat dry with a clean towel or let air dry. Cover the incision with sterile bandages/wound dressing when necessary.

Pain management
In the hospital, immediately following surgery, you will likely be on intravenous (IV) pain medications. Before being sent home from the hospital the IV will be removed and you will be put on prescription and/or over-the-counter pain medication for pain management at home.
Physical activity
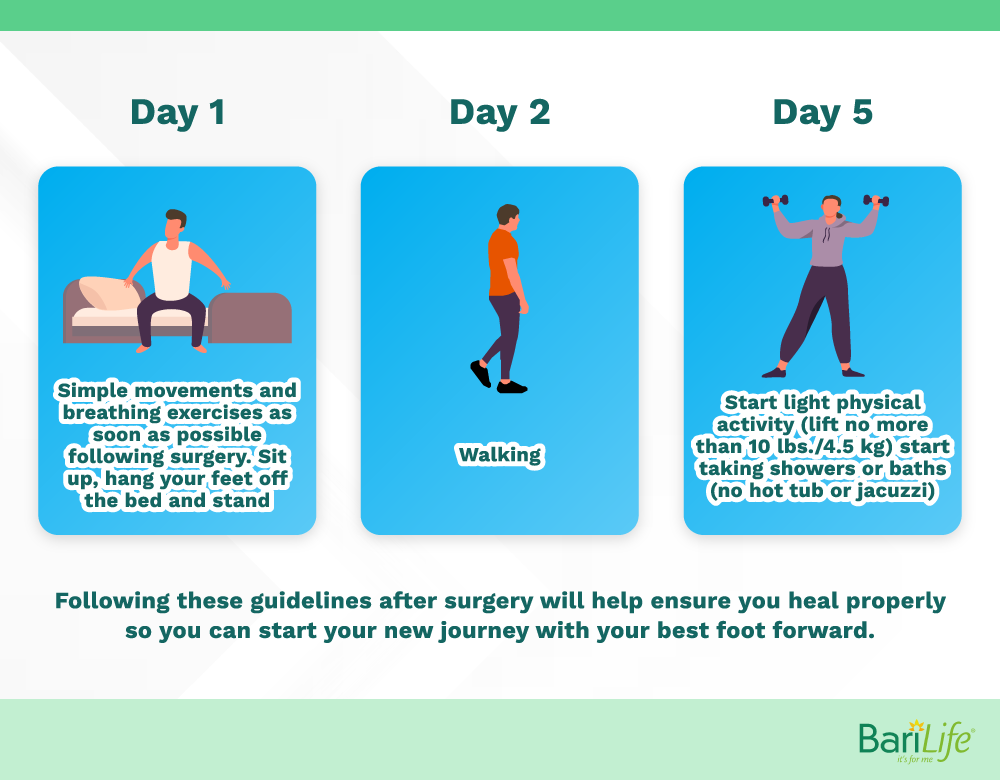
Your level of physical activity should gradually increase over the first week. The first day after surgery you should focus on simple movements while lying in bed. These movements include deep breathing and simple leg movements. Once you know you can accomplish these simple movements you may try to sit on the side of the bed and potentially stand up.
The second day following surgery is when you are likely going to be approved and able to start walking. Walking is very important. Getting up and walking early is an indicator of good long-term outcomes. Sitting, standing, and walking should be done slowly and with the assistance of a physical therapist while in the hospital.
Day 1- Simple movements and breathing exercises as soon as possible following surgery.
Sit up, hang your feet off the bed and stand
Day 2 – walking
Day 5 – Start light physical activity (lift no more than 10 lbs./4.5 kg)
Start taking showers or baths (no hot tub or jacuzzi)
Weeks 2-4
A lot of change will happen between week 2 and week 4 of recovery. Your diet will advance from liquid to pureed and your physical activity will increase allowing you to do more day-to-day tasks. Weight-loss should also begin to appear within the first week or two following surgery.
This time can be both challenging and motivating. You will likely have to challenge yourself to participate in the appropriate amount of physical activity and to follow a strict diet. On the bright side, the first signs of weight loss can often be a strong motivator to keep pushing.
Diet
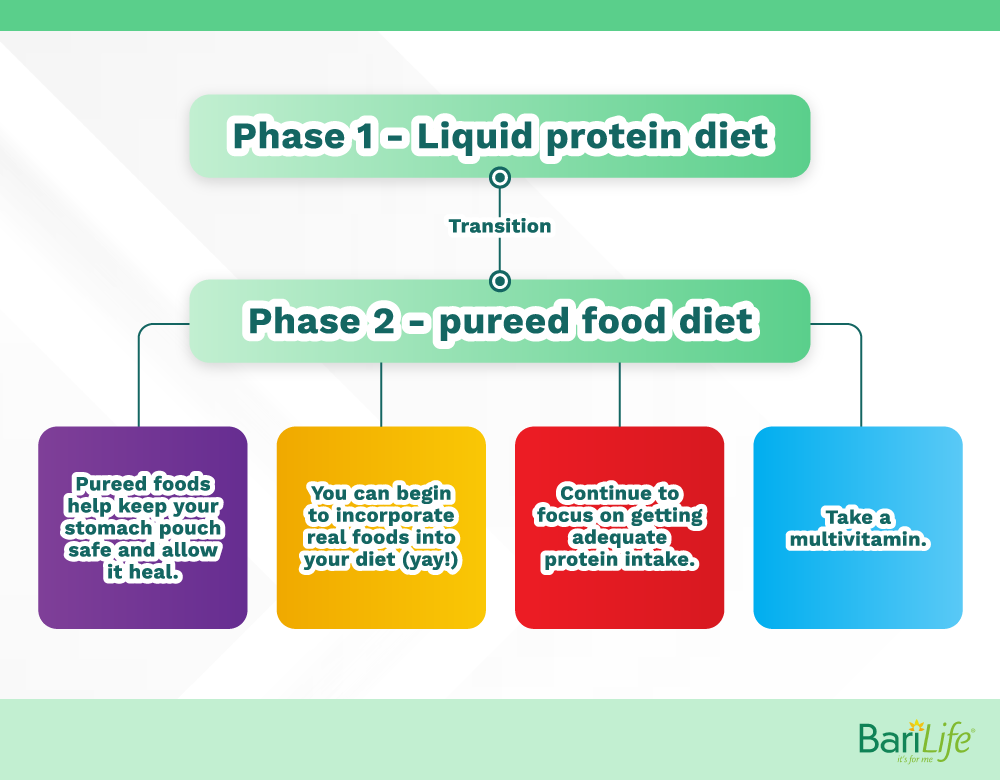
Begin to transition from phase 1 to phase 2 of the 4-phase diet
Phase 1 – Liquid protein diet
Phase 2 – Pureed food diet
Key points of the phase 2 pureed diet:
- Pureed foods help to keep your stomach pouch safe and allow it to heal
- You can begin to incorporate real foods into your diet (yay!)
- Continue to focus on getting adequate protein intake
- Take a multivitamin
As your diet advances, be sure to monitor for signs or symptoms of dumping syndrome. Adjusting your diet and lifestyle can help to improve digestion and reduce side effects.
Wound healing
Incisions should be completely healed after about 2 weeks. Once your incisions are completely healed and closed try to apply lotion frequently to help minimize scarring. If the incision site will be exposed to the sun, make sure to apply sunscreen as this will also help to reduce scarring.
Pain management
You will likely be able to stop taking prescription pain medication after the first week. You may still experience some pain and discomfort after this time, but it can likely be managed by over-the-counter medicine. Most pain should subside after the 2nd or 3rd-week post-op and you likely will not need pain medication of any kind at that point.

Physical activity
If you are no longer taking prescription pain medicine, you will likely be able to begin driving after the first week. Depending on your job you will also likely be able to return to work in the 2–4-week period.

Weeks 4-6
Full recovery takes on average 4-6 weeks barring any complications. This means that your life will begin to look more and more normal during this time period.
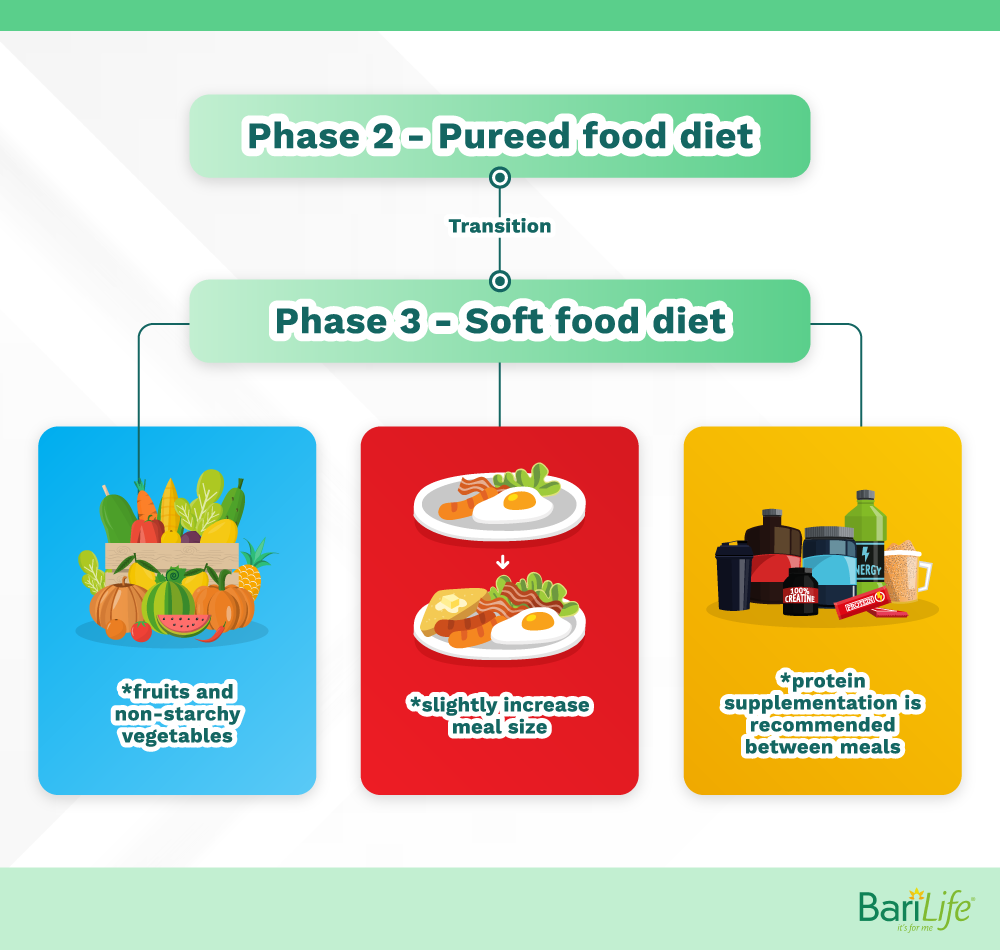
The transition from phase 2 to phase 3
Phase 2 – Pureed food diet
Phase 3 – Soft food diet
On the soft food diet, you will begin to incorporate fruits and non-starchy vegetables into your diet, and you will be able to slightly increase your meal size. Protein supplementation is recommended between meals to help you meet your protein goals.
Physical activity
You should be able to return to most daily activities and some additional exercise, potentially including some heavy lifting. Be sure to talk to your doctor before trying any activity that is very strenuous and/or requires lifting a lot of heavyweights. You will likely need to wait until 6-8 weeks post-op before doing this type of physical activity.
Weeks 6+
After about 6 weeks your life and activity should look pretty normal. You should be approved to do moderate to heavy lifting and most physical activity at this point. You will also transition to what we call the stabilization diet. This diet is the one you should follow long-term.
Diet
The transition from phase 3 to phase 4
Phase 3 – Soft food diet
Phase 4 – Stabilization diet
The stabilization diet will consist of almost all foods including solid foods. Solid foods may need to be reintroduced slowly to allow your body some additional time to tolerate them. Be sure to continue to monitor portion sizes and focus on healthy food consumption.

Wound healing
Your staple line should heal after 6-8 weeks which allows you to incorporate solid foods back into your diet. Although your staple line/gastric pouch is healed, you need to monitor your portion sizes as the gastric pouch can stretch out and can lead to unwanted weight gain.
That a wrap on recovery
Remember these are just general guidelines for recovery. It is so important for you to consult with your bariatric surgeon to see if there are any specific modifications you need to make in your recovery process.
Everyone’s recovery will look different. Do not focus on comparing yourself to others, focus on the daily victories and take the recovery process one step at a time. If you experience severe complications or side effects, be sure to communicate with your team of bariatric health professionals so they can help you to overcome those challenges and get back on track!


What are your tips and tricks to post-bariatric success?