Key Takeaways:
- Bariatric surgery leads to type 2 diabetes remission in the majority of people. Gastric bypass shows the highest success rates.
- The benefits often appear rapidly after surgery, often allowing people to reduce or stop taking their diabetes medication.
- Factors that improve the chances of diabetes remission include having diabetes for less than 5-8 years, being younger, and not requiring insulin therapy.
If you’re living with type 2 diabetes and you struggle with your weight, you’ve probably heard some pretty impressive claims about bariatric surgery. Maybe a friend told you their diabetes “disappeared” after their procedure, or perhaps you’ve seen headlines declaring that weight loss surgery “cures” diabetes. These stories might sound too good to be true—and in some ways, they are.
Does bariatric surgery cure diabetes? The answer isn’t a simple yes or no. It’s more nuanced, and understanding this relationship could be life-changing if you’re considering your options for managing diabetes and obesity.
Let’s delve into what we truly know about bariatric surgery and diabetes, cutting through the hype to uncover the facts that matter for informed health decisions.
Table of Contents
What is Bariatric Surgery?
Before we talk about diabetes, let’s make sure we’re on the same page about what bariatric surgery actually is.
Bariatric surgery (sometimes called weight loss surgery) isn’t just one procedure but a family of operations designed to help people who suffer from severe obesity. These surgeries work by changing your digestive system in ways that limit how much food you can eat, reduce how many nutrients your body absorbs, or both.
Some forms, like gastric bypass, fall into the category of malabsorptive bariatric surgery, which alters the digestive tract in a way that significantly reduces nutrient absorption and can have broad effects on metabolic conditions.
It’s important to understand that bariatric surgery isn’t a quick fix or an easy way out. It’s a serious medical intervention for people whose health is at risk because of their weight, and it requires lifelong changes to diet and lifestyle.
Common Types of Procedures
There are several types of bariatric procedures, but these are the most common:
Gastric Bypass (Roux-en-Y)
During a gastric bypass surgery, your surgeon creates a small pouch from the top of your stomach and links it directly to your small intestine, bypassing most of your stomach and the first section of your small intestine. This means you eat less food, and your body absorbs fewer calories and nutrients as a result.
Think of it like creating a shortcut through your digestive system—food bypasses a significant portion of the normal route, limiting both the amount you can eat and the number of calories you absorb.
Sleeve Gastrectomy
In this type of surgery, about 80% of your stomach is removed, which then leaves a banana-shaped “sleeve.” With a much smaller stomach, you feel full faster and eat less. Unlike gastric bypass, the sleeve doesn’t change how your food is absorbed.
Imagine your stomach is like a large balloon, and the surgery reduces it to something closer to a small tube. You simply can’t fit as much in there anymore, which helps you feel satisfied after eating small portions of food.
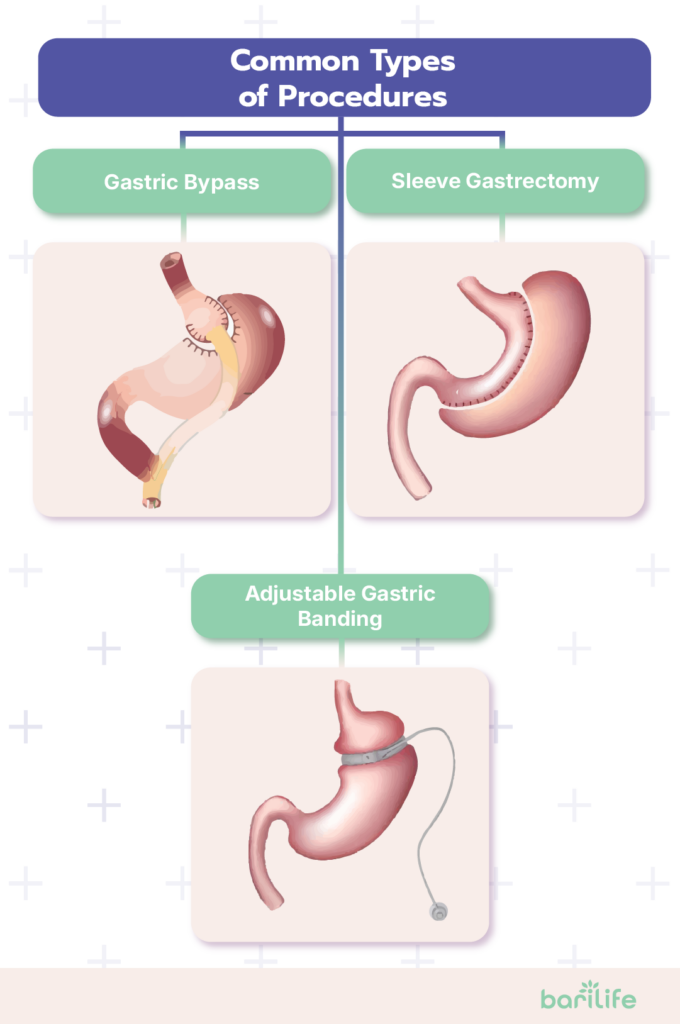
Adjustable Gastric Banding
This less common procedure involves putting an inflatable band around the upper part of your stomach. The band then creates a small pouch just above the band with a narrow entrance to the rest of your stomach. The band can be adjusted to become tighter or looser over time by adjusting the fluid through a port placed under your skin.
It’s like putting an adjustable belt around your stomach that limits how much food you need to eat to feel full.
Eligibility Criteria
Not everyone qualifies for bariatric surgery. Eligible requirements typically include:
- BMI of 40 or higher (severe obesity)
- BMI between 35 and 39.9, and you have serious weight-related health problems like type 2 diabetes, heart disease, or severe sleep apnea
- In some cases, a BMI of 30-34.9 with poorly controlled type 2 diabetes
Most insurance companies and medical centers also require that you try other methods of losing weight first, before you can opt for bariatric surgery.
The Link Between Bariatric Surgery and Diabetes
Now, let’s talk about the connection between weight loss surgery and diabetes, which is truly remarkable. In fact, growing evidence supports the close relationship between bariatric surgery and diabetes remission, making it a highly regarded treatment option for people struggling with both obesity and type 2 diabetes
Improved Glycemic Control
One of the most striking effects of bariatric surgery is how quickly it can improve the blood sugar of patients who have type 2 diabetes. Many patients find their blood sugar readings drop dramatically within days or weeks after surgery, often before they’ve lost much weight.
This rapid improvement suggests something more complex than just weight loss.
Hormonal Changes
The key to understanding how bariatric surgery affects diabetes lies in the hormonal changes that happen after surgery. When portions of your stomach or intestines are bypassed or removed, it changes the production of important gut hormones that control blood sugar, hunger, and metabolism.
For example, after gastric bypass or sleeve gastrectomy, a hormone called GLP-1 typically increases. This hormone helps stimulate insulin production, slow stomach emptying, and signal fullness to your brain. At the same time, hormones that raise blood sugar levels or stimulate appetite often decrease after surgery.
It’s as if your body’s control system for blood sugar gets rewired after bariatric surgery, often becoming significantly more efficient.
Long-Term Benefits
Research shows that these benefits can last for years. Studies comparing bariatric surgery to intensive medical therapy, such as medications and lifestyle changes, consistently show that surgery leads to better diabetes control and higher remission rates in the long term.
For example, one landmark study found that five years after surgery, about half of gastric bypass patients and a third of sleeve gastrectomy patients maintained complete remission of their diabetes, compared to just 5% of patients receiving medical therapy alone.
These kinds of results have revolutionized how we think about treating diabetes in people who also have obesity.
Does Bariatric Surgery Cure Diabetes? Understanding Remission vs. Cure
Now for the big question: Can bariatric surgery cure diabetes? This is where we need to be careful about terminology.
Remission Definition
Medical experts prefer to use the term “remission” rather than “cure” when talking about diabetes after bariatric surgery. Remission means that blood sugar levels return to a healthy range that doesn’t require diabetes medication for control.
According to the American Diabetes Association, complete remission is defined as normal blood glucose levels for at least one year without any diabetes medication. Partial remission means sub-diabetic blood glucose levels without medication for a year.
Think of diabetes remission like cancer remission – the disease isn’t active and doesn’t require treatment, but we can’t guarantee it will never come back.
Remission Rates
So, how likely is it that your diabetes will go into remission after bariatric surgery? The numbers are impressive.
Research shows that about 88% of patients with type 2 diabetes experience complete remission after gastric bypass surgery, with the sleeve gastrectomy showing slightly lower but still significant rates of 50-60%.
One study from the Cleveland Clinic found that about 50% of bariatric surgery patients achieved diabetes remission one year after their procedure. That’s remarkable compared to non-surgical treatments, where remission rates are typically less than 10%.
Factors Influencing Remission
Not everyone has the same chance of achieving diabetes remission after surgery. Several factors affect your likelihood of success:
- Duration of diabetes: The shorter you’ve had diabetes, the better your chances of remission. People who’ve had diabetes for less than 5-8 years have the highest remission rates.
- Diabetes severity: If you’re managing your diabetes with diet and oral medications rather than insulin, you’re more likely to achieve remission after surgery.
- Age: Younger patients typically have higher remission rates than older patients.
- Type of surgery: Procedures that bypass portions of the small intestine (like gastric bypass) generally show higher remission rates than purely restrictive procedures.
- Weight loss success: Greater weight loss after surgery is associated with higher chances of diabetes remission.
If you’ve had diabetes for a long time and take high doses of insulin, your chances of complete remission are lower, but you might still see huge improvements in your blood sugar control.
Can Diabetes Return After Bariatric Surgery?
This is a crucial point that sometimes gets overlooked in discussions about bariatric surgery and diabetes: remission doesn’t always last forever.
Risk of Relapse
Studies tracking bariatric surgery patients over many years have found that diabetes can return in some people, even after initial remission. This doesn’t mean the surgery failed—it just highlights that type 2 diabetes is a complex, chronic disease.

One of the biggest risk factors is weight regain. If you regain significant weight after bariatric surgery, your risk of diabetes returning increases substantially. Other factors associated with relapse include a longer duration of diabetes before surgery, older age, and poor adherence to recommended lifestyle changes.
Long-Term Studies
A landmark 10-year follow-up study tracked diabetes status in patients after bariatric surgery. The results showed that while 75% of patients initially experienced diabetes remission, about a third of those patients experienced a relapse within five years.
However, it’s important to note that even patients who experienced a relapse still had better diabetes control than before surgery. They typically needed fewer medications and had better blood sugar levels than before their operation.
Importance of Lifestyle
This brings us to a critical point: Bariatric surgery isn’t a one-and-done solution for diabetes. The long-term success of surgery depends heavily on your commitment to lifestyle changes afterward.
Maintaining a healthy diet, staying physically active, taking prescribed vitamins and supplements, and attending regular follow-up appointments are all essential to preserving the benefits of surgery and keeping diabetes in remission.
The surgery gives you a powerful tool, but how you use that tool over the years determines your long-term outcomes.
How Does Bariatric Surgery Compare to Other Diabetes Treatments?
If you’re weighing your options for managing diabetes, you’re probably wondering how bariatric surgery stacks up against traditional treatments.
Effectiveness
When it comes to achieving diabetes remission, bariatric surgery outperforms medical therapy by a wide margin. Multiple randomized controlled trials have shown that surgery is much more likely to result in diabetes remission than even the most intensive medication and lifestyle interventions.
For example, a 12-month study showed that 42% of gastric bypass patients and 37% of sleeve gastrectomy patients achieved complete diabetes remission after one year, compared to just 12% of patients receiving intensive medical therapy.
The difference becomes even more pronounced over time. After five years, about half of surgery patients maintained significant improvement in blood sugar control, compared to just 5% of those treated with medications and lifestyle changes alone.
Sustainability
Bariatric surgery also appears to offer more sustainable improvements in diabetes control. While medications can effectively lower blood sugar, they typically need to be continued indefinitely and often need to be increased over time as diabetes progresses.
In contrast, many bariatric surgery patients experience long-term improvements in insulin sensitivity and beta-cell function, allowing for reduced medication needs or even complete remission for years.
This sustainability is one of the most compelling arguments for considering surgery as a diabetes treatment.
Risks and Considerations
Of course, surgery isn’t without risks. Short-term complications can include bleeding, infection, blood clots, and leaks in the surgical connections. Long-term risks include nutritional deficiencies, bowel obstruction, hernias, and the potential need for revision surgery.
Additionally, bariatric surgery requires a lifelong commitment to dietary changes, vitamin supplementation, and regular medical follow-up. Not everyone is prepared for or interested in these permanent lifestyle modifications.
Medications and lifestyle changes, while less effective at achieving remission, carry different risk profiles and may be more appropriate for certain patients based on their preferences, health status, and goals.
Can Bariatric Surgery Become a Standard Diabetes Treatment?
Given the impressive results of bariatric surgery for diabetes, you might wonder if it could eventually become a standard treatment option, even for people who aren’t severely obese.
Current Guidelines
Current medical guidelines have already begun to recognize bariatric surgery as a treatment for diabetes, not just for weight loss. The American Diabetes Association now includes metabolic surgery in its treatment algorithm for type 2 diabetes, particularly for patients who have a BMI of 35 or higher.

Some guidelines have even lowered the BMI threshold to 30 (or as low as 27.5 for Asian populations) for patients with poorly controlled type 2 diabetes, acknowledging that the metabolic benefits of surgery may justify its use in patients with less severe obesity.
Ongoing Research
Research continues to explore the potential of bariatric/metabolic surgery for a wider range of patients with diabetes. Scientists are studying the mechanisms behind diabetes remission after surgery, looking for ways to predict which patients will benefit most, and developing less invasive procedures that might provide similar benefits with lower risks.
Some researchers are even investigating whether the hormonal changes that occur after bariatric surgery could be replicated with medications or less invasive procedures, potentially bringing the benefits to more patients without major surgery.
Individualized Approach
Despite the promising research, bariatric surgery isn’t right for everyone with diabetes. The decision to pursue surgery should always be individualized, taking into account:
- Your overall health and surgical risk
- The severity and duration of your diabetes
- Your willingness to commit to post-surgical lifestyle changes
- Your personal preferences and values
- The availability of expert surgical and support teams in your area
For some people with type 2 diabetes, especially those with obesity and poor diabetes control despite other treatments, bariatric surgery might be the most effective option. For others, a combination of medications, diet, and lifestyle changes might be more appropriate.
Conclusion
Let’s circle back to our original question: Can bariatric surgery cure diabetes? The most accurate answer is that it can lead to long-term remission in many patients, which is the closest thing we currently have to a cure for type 2 diabetes.
While not a guaranteed permanent cure, bariatric surgery offers the highest rate of diabetes remission of any current treatment. For many people, it provides years of life without diabetes symptoms or medications—an outcome that would have seemed impossible just a few decades ago.
If you’re living with both type 2 diabetes and obesity, it’s worth having a conversation with your healthcare team about whether bariatric surgery might be an option for you. The procedure isn’t a magic solution, and it requires significant lifestyle changes and a long-term commitment. Still, for many people, it offers a path to diabetes remission that medication alone cannot provide.
Each person’s situation is unique, and what works for one person might not be right for another. The most important thing is to work with healthcare providers who understand both diabetes and bariatric surgery to develop a treatment plan that aligns with your health needs and personal goals.
Whether bariatric surgery is part of your diabetes management plan or not, the key to long-term health always includes healthy eating, regular physical activity, and ongoing medical care. These fundamentals remain important no matter which treatment path you choose.
How Bari Life Can Help
Proper nutrition is crucial for maintaining the metabolic benefits of bariatric surgery, especially for patients with type 2 diabetes. Bari Life offers a wide range of bariatric vitamins and supplements specifically formulated to support your post-operative nutritional needs.
Our products include bariatric multivitamins, available in both chewable bariatric vitamins and liquid bariatric vitamin forms to ensure easy absorption and convenience. For those requiring additional iron support, we also provide a bariatric multivitamin with iron, ideal for maintaining energy levels and preventing anemia.
Bari Life’s comprehensive product line extends beyond just vitamins. We offer high-quality bariatric protein shakes and bariatric protein bars that are great for meeting your protein goals without excess sugar or calories. These options are designed to help stabilize blood sugar levels, making them an excellent choice for individuals managing type 2 diabetes.
To complement your diet, our selection of bariatric snacks ensures you have healthy, portion-controlled options at your fingertips. Additionally, bariatric calcium chews help support bone health—a crucial aspect of recovery and long-term wellness post-surgery.
For digestive health, we recommend incorporating a bariatric probiotic into your routine, as it promotes gut balance and may aid in better nutrient absorption. Bari Life also addresses one of the common concerns following surgery with our specialized bariatric vitamins for hair loss, helping to maintain healthy hair growth through proper nutrition.
Visit Bari Life today to discover how our complete bariatric vitamin formulations can support your journey toward diabetes remission and better overall health after weight loss surgery.
If you want to learn more, why not check out these articles below:
- PCOS and Bariatric Surgery
- Best Bariatric Surgery For Hiatal Hernia
- Bariatric Surgery For Hypertension
- Bariatric Surgery For GERD
- Bariatric Surgery and Gallbladder
Resources
Holst, J. J., & Madsbad, S. (2021). What is Diabetes Remission? Diabetes Therapy.



What are your tips and tricks to post-bariatric success?