Finally, you’re losing weight. After countless diets and torturous exercise routines, weight loss surgery has given you hope.
Your blood sugar and cholesterol levels are also looking better. At last you’ve found the solution to achieving a healthy weight and a sense of well-being.
Unfortunately, along with the benefits it offers, bariatric surgery also has some potential complications. One of the biggest issues is poor nutrient absorption, which is why taking the best bariatric vitamins is crucial to maintaining proper nutrient levels post-surgery.
In this article, we’ll first explore the link between the different types of bariatric surgery and vitamin deficiencies. Then, we will unravel the risks involved and how to prevent them through regular monitoring, supplementation, and a balanced diet.
Table of Contents
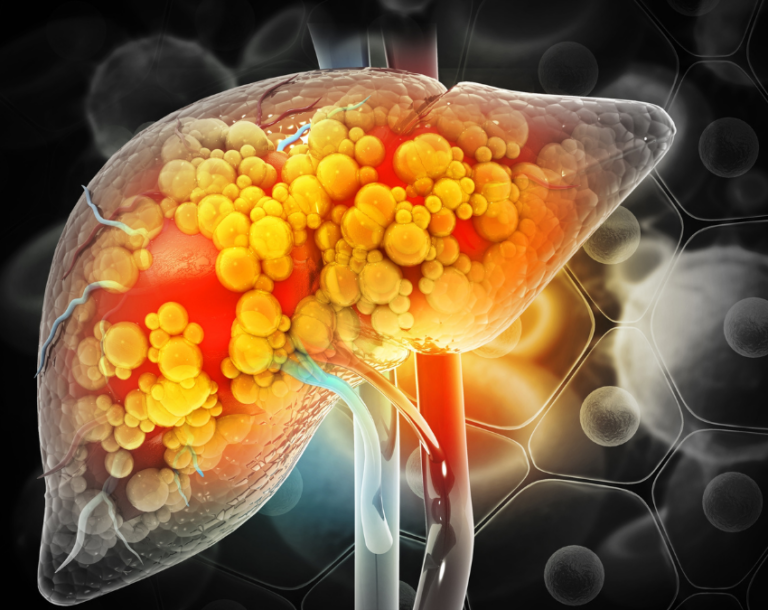
Understanding Vitamin Deficiencies Post-Bariatric Surgery
Changing the structure of your digestive system also changes its function. That’s why people who have had weight loss surgery experience certain vitamin and mineral deficiencies. To address these deficiencies, it’s important to take the best bariatric vitamins all-in-one so you get all the nutrients you need.
Some of the most common nutritional deficiencies after bariatric surgery include:
- Thiamin: Low levels of thiamin (vitamin B1) are often seen 4-6 weeks after surgery in about 30% of patients.
- Folate: On average, 38% of bariatric patients experience folate deficiency which often develops unnoticed in the first year post surgery.
- Vitamin B12: Up to 62% of patients experience vitamin B12 deficiency, with rates rising 5 years after the operation.
- Vitamin D: Over 50% of bariatric patients are deficient in vitamin D. 10 years after surgery this number climbs to 65%. It’s important to take Vitamin D3 since it’s the best vitamin D for bariatric patients.
- Calcium: Low levels of calcium are seen in about 10% of bariatric patients.
- Iron: Up to 45% of people who have had bariatric surgery are iron deficient.
- Copper: It is estimated that copper deficiency occurs in 4-18% of bariatric patients.
- Zinc: After 18 months, 20-24% of weight loss surgery patients have an iron deficiency.
Not everyone will experience vitamin deficiency after bariatric surgery. Your supplement regime, dietary intake, and type of surgery influence your risk of developing low levels of certain micronutrients.
Let’s take a look at which nutrients are affected by three of the most common bariatric procedures:
Roux-en-Y Gastric Bypass (RYGB)
The “gold standard” of bariatric surgery, Roux-en-Y gastric bypass, involves creating a small pouch using the upper part of your stomach and connecting it to the small intestine at the Roux limb, bypassing a large part of the small intestine.
This changes the way you digest food, leading to weight loss. Unfortunately, it also alters the absorption of nutrients including vitamin B12, folate, thiamin, iron, calcium, and vitamin D.
Vertical Sleeve Gastrectomy (VSG)
Generally referred to as gastric sleeve surgery, this procedure removes a large portion of your stomach, leaving a “sleeve-shaped” organ that looks like a banana.
Vitamin deficiencies are less common after gastric sleeve surgery. Yet, iron and vitamin B12 are often low post surgery. It is also crucial to monitor calcium and vitamin D levels.
Biliopancreatic Diversion (BPD)
Similar to a gastric sleeve, a large portion of your stomach is removed during a biliopancreatic diversion. The remaining “sleeve” is then connected to the small intestine, bypassing the initial section.
The result is successful weight loss at the cost of your nutritional status. Digestion and absorption are impaired causing the same nutrient deficiencies as gastric bypass surgery—only worse.
Symptoms and Health Risks of Vitamin Deficiencies
Dietary restrictions along with inadequate supplementation combine to cause bariatric surgery nutritional deficiencies. Your healthcare team will closely monitor you for any symptoms of vitamin and mineral inadequacies to avoid potential health risks.
For this reason, it’s important to use the best bariatric vitamins after surgery to prevent these section of the small intestine–the part bypassed by several bariatric procedures. kinds of deficiencies.
Thiamin deficiency, called “bariatric beriberi,” occurs because the vitamin is absorbed in the first.
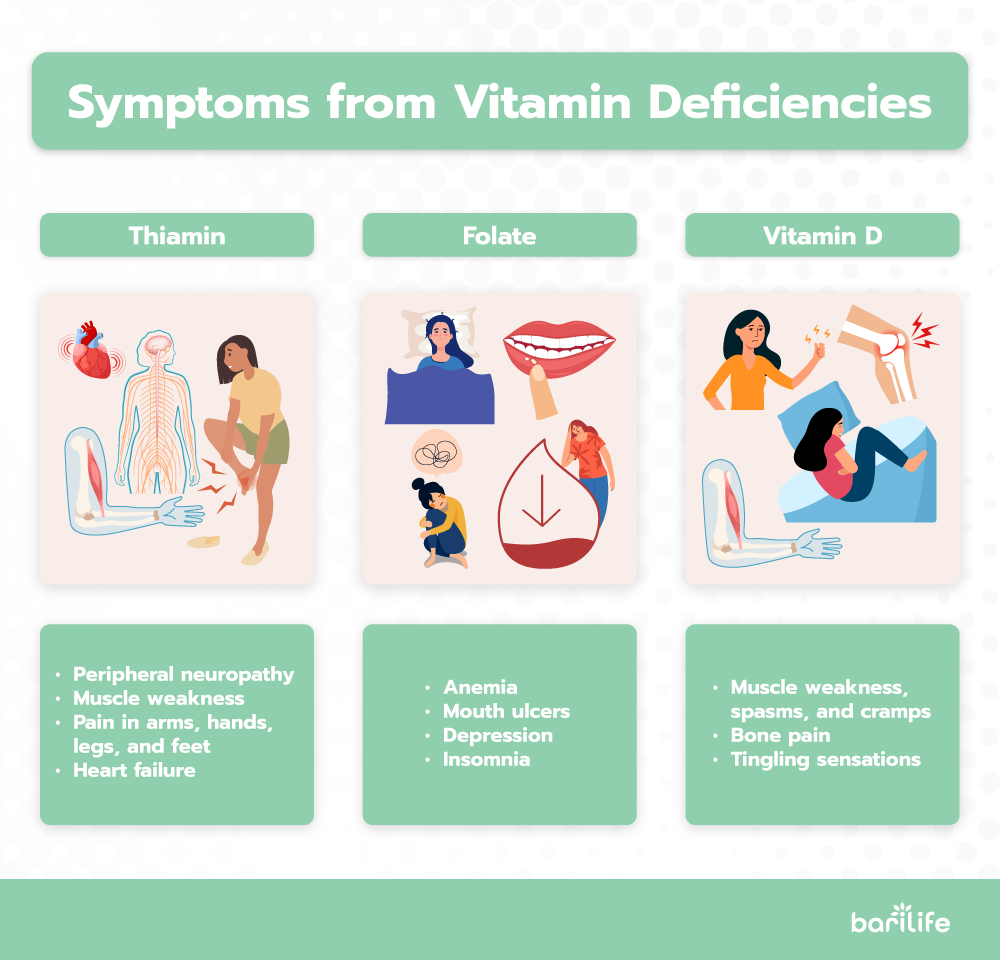
Early signs of thiamin deficiency include:
- Peripheral neuropathy
- Muscle weakness
- Pain in arms, hands, legs, and feet
- Heart failure
- Edema
- Difficulty breathing
- Nausea
- Vomiting
- Constipation
If left untreated, the condition can evolve into Wernicke encephalopathy. Symptoms include eye muscle paralysis, uncontrolled eye movements, poor muscle control, confusion, and short-term memory loss.
Hallucinations and psychosis can also occur. In this case the condition is referred to as Wernicke-Korsakoff syndrome or Korsakoff psychosis.
Folate deficiency shares many symptoms with vitamin B12 deficiency. When your levels of folic acid (folate) are low, you may experience:
- Fatigue.
- Painful inflamed tongue.
Megaloblastic anemia and pancytopenia (low levels of all types of blood cells) are long term complications that can be avoided by the right supplementation.
Vitamin B12 deficiency occurs after most types of bariatric surgery, but is worse after RYGB. Signs of low vitamin B12 include:
- Fatigue
- Dizziness
- Sore tongue
- Shortness of breath
- Loss of appetite
- Diarrhea
- Heart palpitations
- Ringing in the ears
- Numbness and tingling in the hands and feet
When low vitamin B12 levels are left unchecked, you might develop neurological symptoms such as psychosis, irritability, forgetfulness, and dementia.
Vitamin D deficiency affects calcium levels in your body as it is involved in the absorption of this mineral and how it is used. Common signs of low vitamin D levels include:
- Muscle weakness, spasms, and cramps
- Bone pain
- Tingling sensations
If left unmanaged, low levels of vitamin D can cause softening of the bones (osteomalacia) or weak, brittle bones (osteoporosis).
Calcium deficiency is closely related to vitamin D deficiency, and shares the same early signs and long-term complications.
Iron deficiency is very common after bariatric surgery, especially in women. Signs that your iron levels are low include:
- Fatigue
- Difficulty concentrating
- Difficulty swallowing
- Weak immune system
Inadequate iron intake and absorption leads to iron-deficiency anemia, damage to the small intestine, concave nails (koilonychia), and a swollen tongue (glossitis).
Copper deficiency can result in issues with your hair, skin pigmentation, immune system, and blood cell production. Long-term, low levels of this mineral may cause anemia, leukopenia (low levels of disease-fighting leukocytes), neutropenia (low levels of white blood cells), thrombocytopenia (low platelet count), and pancytopenia (low levels of platelets and red and white blood cells).
Zinc deficiency symptoms include altered sense of taste, skin rashes, and lesions. Long-term complications may be a weakened immune system, changes to reproductive hormones, hair loss, poor wound healing, and diarrhea.
Importance of Regular Monitoring and Blood Tests
Vitamin deficiency in bariatric patients is a common problem. That’s why the American Society for Metabolic and Bariatric Surgery (ASMBS) recommends routine screening for the most common bariatric surgery nutritional deficiencies:
- Thiamin: High risk patients—women, people of African descent, patients with gastrointestinal symptoms and chronic health conditions–must be tested within the first 6 months after surgery, and every 3-6 months after.
- Folate: Recommended for all patients and should be included in the best vitamins for hair loss after bariatric surgery
- Vitamin B12: Recommended for all weight loss surgery patients. If you take medication such as metformin or proton-pump inhibitors that are known to affect your vitamin B12 status, more regular screening is recommended—every 3 months.
- Vitamin D and Calcium: Recommended for all bariatric patients.
- Iron: Your iron status must be checked within 3 months of your surgery, and then, every 3-6 months for the first year. Thereafter, annual screening is recommended.
- Copper: Test your zinc levels at least once a year–even if you don’t have symptoms of deficiency.
- Zinc: If you’ve had RYGB or BPD surgery your zinc levels will be screened annually. They will also be checked if you have symptoms of anemia and your iron levels are not low.
Because nutrient deficiencies can creep up on you without any noticeable signs, it is critical to work closely with your healthcare team to ensure the best weight loss and health outcomes post-surgery.
Effective Supplementation Strategies
our bariatric healthcare team has you covered. What’s more, you can take advantage of the supplements designed specifically for people who’ve had weight loss surgery. They are formulated with higher doses to meet your unique needs and are available in forms your body can use.
You might also ask, do vitamin patches work for bariatric patients? The effectiveness of these patches can vary, and it’s generally recommended to stick to oral supplements unless otherwise advised by your doctor.
Seeing as it’s a lifelong commitment, taking your supplements needs to be as simple as possible. While you could take a separate product for each nutrient, an all-in-one multivitamin, such as Bari Life’s bariatric vitamins chewable, Just One, makes more sense.
It is available in tablet or chewable form so you can choose the one that works best for you. Remember, liquids, chewables, and tablets that dissolve under the tongue are best tolerated post bariatric surgery.
You will also have to take a separate calcium supplement to meet your increased requirements. Barilife has a tasty chewable option for you in their flavored Bariatric Calcium Chews.
Dietary Adjustments to Support Nutrient Intake
Your vitamin supplements are key to maintaining healthy levels of micronutrients after having weight loss surgery. But your diet is just as important.
Work closely with a registered dietitian. They can help by creating a personalized nutrition plan that incorporates high-protein foods, fortified foods, and nutrient-dense vegetables, ensuring your energy and vitamin needs are met.
It also helps to arm yourself with a collection of tasty and well-tolerated recipes.
Long-Term Management and Lifestyle Changes
The road to post-bariatric surgery success is paved by a long-term commitment to nutritional health and supplementation. It also pays to develop other healthy lifestyle habits like regular exercise, drinking enough water, and effective stress management.
Routine screening ensures that nutrient deficiencies due to dietary restrictions and poor absorption are detected early. Taking the right supplements can treat your symptoms and prevent further complications.
Finally, stay informed and motivated. Take advantage of ongoing education opportunities and support groups for bariatric patients. You are navigating some pretty big changes, but you don’t have to do it alone.
Conclusion
While bariatric surgery can lead to significant weight loss and improved health, it also increases the risk of nutrient deficiencies due to changes in the digestive system. Regular monitoring, blood tests, and proper supplementation are essential to prevent complications. Bari Life’s Just One multivitamin and Bariatric Calcium Chews offer convenient solutions tailored to the needs of bariatric patients. With ongoing healthcare support, dietary adjustments, and lifestyle changes, patients can maintain their health and prevent deficiencies after surgery.



What are your tips and tricks to post-bariatric success?