Key Takeaways:
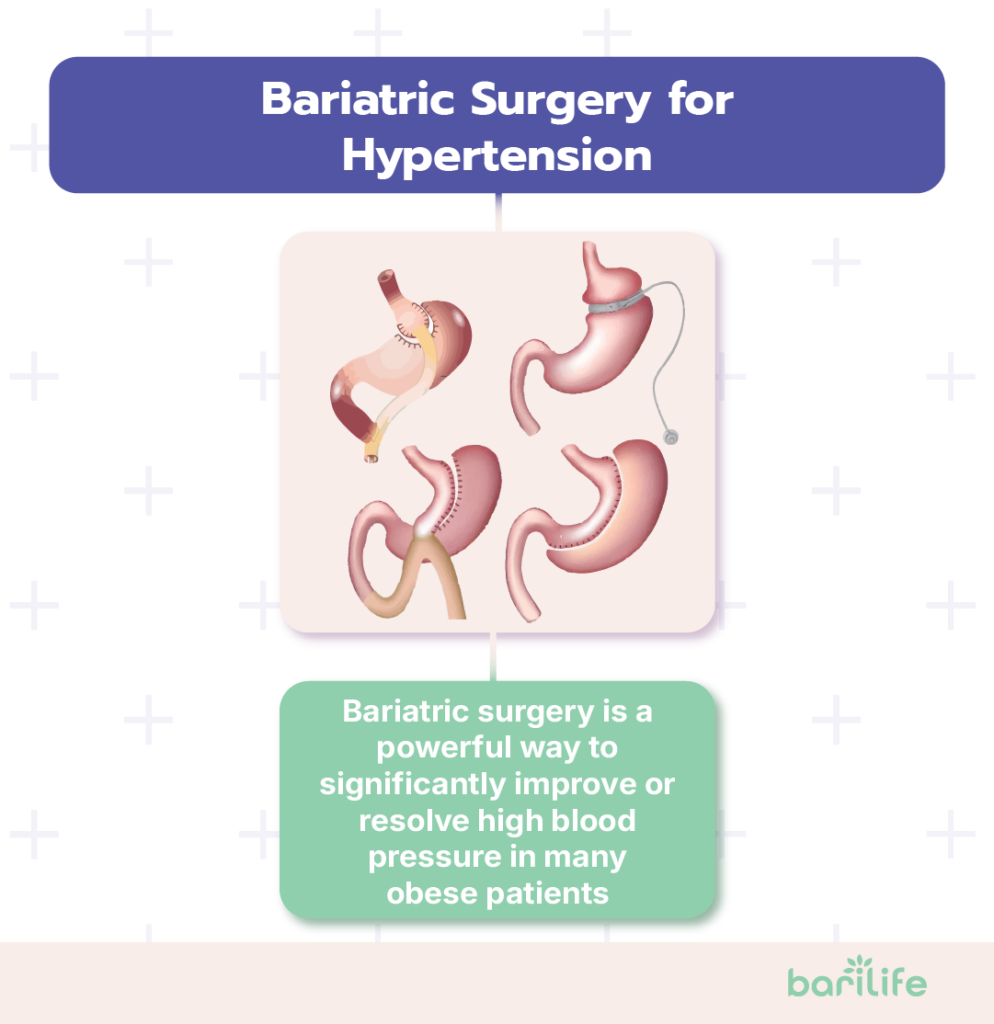
- Bariatric surgery can significantly improve or even resolve high blood pressure in many individuals with obesity, often reducing the need for medication.
- The procedure’s effects go beyond weight loss, involving hormonal shifts, reduced abdominal pressure, and improved conditions like sleep apnea.
- While the potential health benefits are substantial, bariatric surgery requires a lifelong commitment to dietary, lifestyle, and medical follow-up changes to ensure lasting success.
If you’re dealing with both excess weight and high blood pressure, you’re not alone. These two health challenges often go hand-in-hand, making everyday life more difficult while increasing your risk of serious health problems in the future. But what if there were a solution that could help with both issues?
Bariatric surgery for hypertension is becoming increasingly recognized as an effective option for people struggling with both obesity and high blood pressure. But is it right for you? Let’s look at what the science says about how weight loss surgery affects your blood pressure, who might benefit from it, and what you can expect if you choose this path.
Table of Contents
Understanding Hypertension in Obese Patients
Before we talk about surgery, let’s get clear on why excess weight and high blood pressure are so closely connected.
The Weight-Blood Pressure Connection
When you’re carrying extra weight, your chances of developing high blood pressure go up significantly. The heavier you are, the more likely you are to have high blood pressure. Your body is working harder when you’re carrying extra weight, and that extra work affects your circulatory system.
What’s Happening Inside Your Body
So, what exactly happens inside your body to raise your blood pressure when you gain weight? Several things:
First, your heart has to work harder to pump blood through additional blood vessels that form to supply oxygen and nutrients to your extra tissue. This increased workload can lead to a gradual rise in blood pressure over time.
Second, excess fat cells don’t just sit there—they’re actually active, releasing hormones and other substances that can directly affect your blood pressure.
Third, excess weight often leads to insulin resistance, which can cause your kidneys to retain sodium and water, increasing blood volume and pressure.
Why It Matters
High blood pressure may not cause noticeable day-to-day symptoms, but over time, it silently damages your blood vessels and organs. When you have both obesity and hypertension, your risk of serious complications goes up dramatically, including:
- Heart attacks
- Strokes
- Heart failure
- Kidney damage
- Vision problems
- Cognitive decline
The great news is that losing weight can significantly improve your blood pressure. Even a minor weight loss can make a difference, but the substantial weight loss that comes with bariatric surgery often produces dramatic improvements.
How Bariatric Surgery Affects Hypertension
When it comes to treating high blood pressure in people with obesity, bariatric surgery has shown some impressive results. These results are not just limited to blood pressure—patients often see improvements in other obesity-related conditions, including bariatric surgery for GERD, which targets acid reflux, another common comorbidity.
The Blood Pressure Effect
Studies consistently show that bariatric surgery for high blood pressure leads to significant improvements. About 60-70% of patients who had hypertension before surgery find that their blood pressure returns to the normal range afterward, often allowing them to reduce or eliminate the medications they were taking.
What’s remarkable is how quickly these changes can happen. While some blood pressure improvement comes with weight loss over time, many patients notice changes in their readings within days or weeks after surgery, well before they’ve lost a significant amount of weight.
Beyond Just Weight Loss
So why does bariatric surgery have such a powerful effect on blood pressure? Several other mechanisms come into play:
Hormonal Changes
After bariatric surgery, the way your body produces and responds to various hormones changes dramatically. Gut hormones like GLP-1 increase, while hormones that can raise blood pressure decrease. These hormonal shifts can enhance insulin sensitivity and reduce inflammation throughout the body, both of which contribute to lowering blood pressure.
Reduced Abdominal Pressure
The fat around your midsection (visceral fat) puts physical pressure on your kidneys and blood vessels. When this fat is reduced after surgery, that physical pressure decreases, allowing your kidneys to function better and your blood vessels to relax.
Improved Sleep Apnea
Many people with obesity have sleep apnea, which contributes to high blood pressure. As weight drops after surgery, sleep apnea often improves or resolves completely, helping normalize blood pressure.
Changes in Gut Bacteria
Research suggests that bariatric surgery actually changes the mix of bacteria in your digestive system. These changes may affect your metabolism and blood pressure regulation.
Long-Term Benefits
One of the most important questions about any treatment is, “Will the benefits last?” The research on bariatric surgery for hypertension is encouraging.
Studies following patients for 5-10 years after surgery show that most maintain significant improvements in blood pressure, even if they regain some weight. One large study found that 10 years after surgery, patients were half as likely to be taking blood pressure medications compared to similar patients who didn’t have surgery.
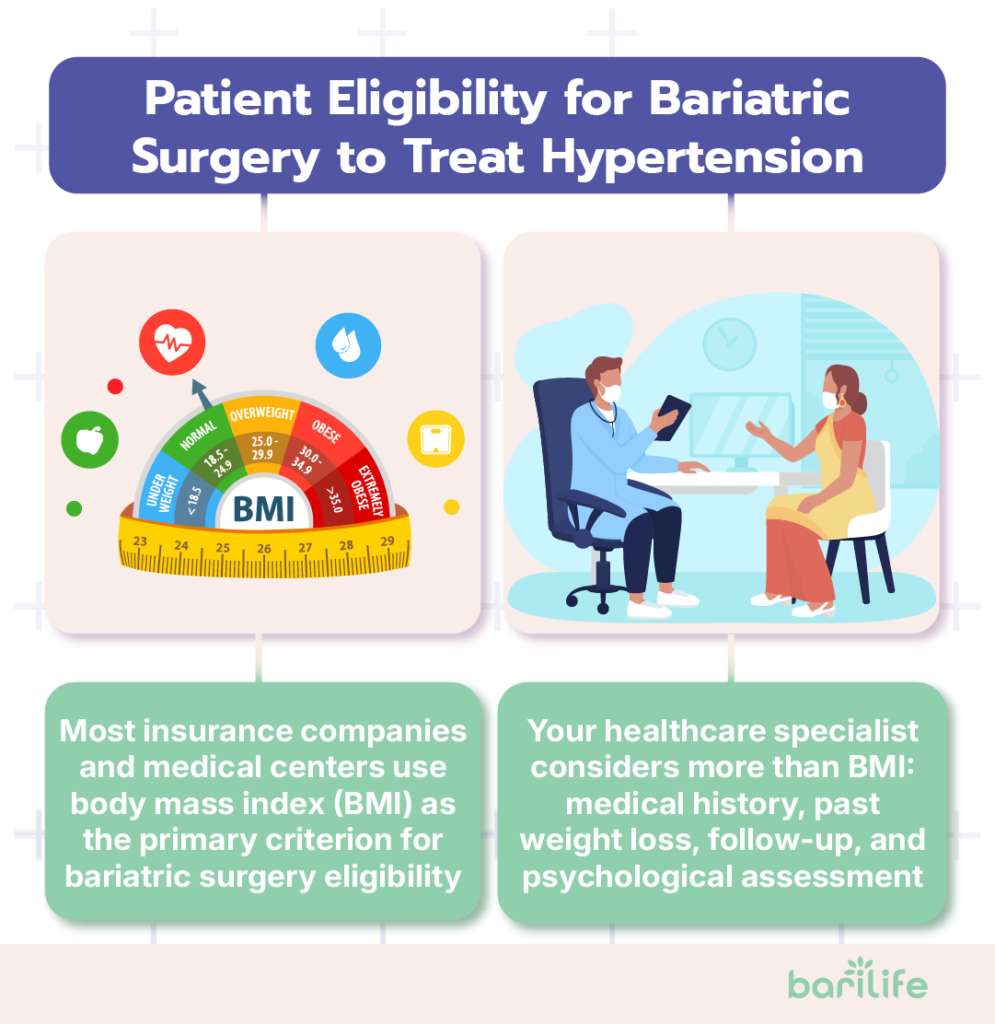
Patient Eligibility for Bariatric Surgery to Treat Hypertension
So, how do you know if you might be a good candidate for using bariatric surgery to address your high blood pressure? Here’s what medical guidelines suggest:
BMI Requirements
Currently, most insurance companies and medical centers use body mass index (BMI) as the primary criterion for bariatric surgery eligibility:
- If your BMI is 40 or higher, you may qualify regardless of whether you have high blood pressure or other weight-related conditions.
- If your BMI is between 35 and 40, you typically need to have at least one obesity-related health condition, like hypertension, type 2 diabetes, or sleep apnea.
- Some centers now consider patients with BMIs between 30 and 35 who have poorly controlled metabolic conditions, but this is less common and often not covered by insurance.
Medical Evaluation
Beyond BMI numbers, determining if you’re a good candidate for surgery involves a comprehensive evaluation:
- Medical history: Your doctors will review your blood pressure history, how well it’s controlled with medications, and whether you have other health conditions that might affect surgical outcomes.
- Previous weight loss attempts: Most programs require documentation that you’ve tried other weight loss methods without long-term success.
- Psychological evaluation: This helps ensure you understand the lifestyle changes required after surgery and don’t have untreated mental health conditions that could interfere with post-operative success.
- Commitment to follow-up: Bariatric surgery isn’t a one-and-done solution – it requires lifelong follow-up care. Your healthcare team will assess your ability and willingness to maintain long-term medical care.
Age Considerations
While there’s no strict upper age limit for bariatric surgery, the risks and benefits must be carefully weighed for older adults. Most patients are between 18 and 65 years old, but suitable candidates outside this range can be considered on an individual basis.
For adolescents with severe obesity and hypertension, bariatric surgery may be considered when:
- They have reached physical maturity (typically age 13+ for girls and 15+ for boys)
- They have a BMI over 40 with serious health conditions or over 50 regardless of other conditions.
- They demonstrate an understanding of the required lifestyle changes and have family support
These considerations help identify patients most likely to benefit from surgery while minimizing risks.
Risks and Considerations
Like any surgical procedure, bariatric surgery comes with possible risks that should be carefully considered in relation to its benefits for blood pressure control.
Surgical Risks
The risks of bariatric surgery have decreased significantly over the years as techniques have improved, but they still include:
Short-Term Complications
- Infection at the surgical site or within the abdomen
- Bleeding
- Blood clots
- Leaks in the surgical connections
- Breathing problems
- Adverse reactions to anesthesia
Long-Term Complications
- Nutritional deficiencies (especially vitamins D, B12, iron, and calcium)
- Gallstones
- Hernias
- Strictures or bowel obstructions
- Dumping syndrome (rapid emptying of stomach contents)
- Potential need for revision surgery
Your personal risk depends on factors like age, other health conditions, and the specific procedure you undergo.
Lifestyle Commitment
Perhaps the biggest consideration isn’t the surgery itself but the lifelong changes required afterward:
Dietary Changes
You’ll need to:
- Eat much smaller meals
- Focus on protein-rich foods
- Avoid high-sugar, high-fat foods
- Take vitamin and mineral supplements daily
- Separate eating and drinking
Physical Activity
Regular exercise becomes essential for:
- Maximizing weight loss
- Maintaining lost weight
- Supporting cardiovascular health
- Further improving blood pressure
Medical Follow-Up
Lifelong monitoring includes:
- Regular blood pressure checks
- Blood tests for nutritional status
- Annual visits with your bariatric team
- Ongoing medication adjustments as needed
These commitments require significant lifestyle adjustments and discipline. The most successful patients view surgery not as a quick fix but as a tool that, when combined with lifestyle adjustments, can lead to lasting improvements in health.
Psychological Factors
The psychological aspects of bariatric surgery are just as important as the physical ones:
- Body image changes: Rapid weight loss can result in significant changes in appearance, including loose skin. Adjusting to your “new body” can be emotionally challenging.
- Transfer addiction risk: Some patients find that after surgery, they transfer their relationship with food to other potentially problematic behaviors like alcohol use, shopping, or gambling.
- Depression and anxiety: While many patients experience improved mental health after surgery, others may struggle with adjustment issues or depression, particularly if they had expectations that surgery would solve all their problems.
- Relationship changes: As your body and lifestyle change, relationships with partners, family, and friends may also change in unexpected ways.
Post-Surgery Lifestyle and Blood Pressure Management
If you decide that bariatric surgery is right for you, how can you maximize your chances of long-term blood pressure improvement? Here’s what successful patients do.
Dietary Approaches for Blood Pressure Control
After surgery, your diet will change dramatically out of necessity (your stomach is much smaller), but you can make specific food choices that support healthy blood pressure:
- Focus on potassium-rich foods: Fruits and vegetables like bananas, sweet potatoes, spinach, and avocados help counter the effects of sodium.
- Limit sodium intake: Processed foods are often high in sodium, which can raise blood pressure. Learning to cook fresh foods using herbs and spices instead of salt can make a huge difference.
- Stay hydrated: Drinking enough water (separate from meal times) helps maintain proper blood volume and supports kidney function.
- Consider the DASH approach: The Dietary Approaches to Stop Hypertension (DASH) eating pattern has been proven to lower blood pressure. Many of its principles can be adapted to post-bariatric eating.
Activity and Exercise
Physical activity is a useful tool for managing blood pressure after bariatric surgery. Even walking for 10-15 minutes several times a day can provide benefits when you are just starting out.
As your fitness improves, aim to engage in at least 150 minutes of moderate exercise per week, in addition to strength training exercises twice a week.
Whether it’s dancing, swimming, cycling, or gardening, the best exercise is the one you’ll actually do consistently. Many patients find that seeing improvements in their fitness level provides motivation to continue.
Exercise is not only great for managing weight, but it also improves blood vessel health.
Medication Management
Most patients find that their blood pressure medication needs to change after surgery. Even if your blood pressure readings improve dramatically, you want to always consult with your doctor before changing your medication routine.
Monitoring your blood pressure at home can help you keep track of changes. This can help your doctor adjust medications appropriately. Also, some bariatric procedures change how medications are absorbed, so your doctor might need to adjust dosages or switch to different formulations.
Conclusion
Bariatric surgery for high blood pressure offers a powerful intervention that can significantly improve or even resolve hypertension in many obese patients. The benefits extend beyond lower blood pressure readings. It also reduces cardiovascular risk and improves the quality of life.
However, surgery is a significant step that requires consideration of both the potential benefits and the lifelong changes that follow. The decision should be made in partnership with healthcare providers who can help explain your individual risks and likely outcomes.
If you’re struggling with both obesity and hypertension despite your best efforts with diet, exercise, and medications, it may be worth discussing bariatric surgery with your doctor.
How Bari Life Can Help
Managing your nutrition properly after bariatric surgery is essential for maintaining both your weight loss and blood pressure improvements. Bari Life offers specialized bariatric vitamins and supplements that support overall cardiovascular health while preventing the nutritional deficiencies that commonly occur after surgery.
Our wide range of bariatric multivitamins, including bariatric multivitamin with iron options, ensures you get the critical nutrients your body needs in the most absorbable forms. For those who prefer flexibility, we also offer bariatric vitamins chewable and liquid bariatric vitamin formulations, making it easier to stay consistent with your post-op regimen.
To support your protein intake and muscle maintenance, Bari Life provides delicious bariatric protein shakes and bariatric protein bars, perfect for on-the-go nutrition that doesn’t compromise on taste or quality. These options complement our nutritious bariatric snacks, designed to satisfy cravings while staying aligned with your health goals.
In addition to essential vitamins and proteins, Bari Life also offers bariatric calcium chews and bariatric probiotic supplements to enhance digestive and bone health—both crucial after weight loss surgery. And for those experiencing hair thinning or loss, our bariatric vitamins for hair loss are specially formulated to help support hair strength and regrowth.
Visit Bari Life today to discover how our complete bariatric vitamin formulations, snacks, and supplements can help support your journey to better heart health and blood pressure control after weight loss surgery.
If you want to learn more, why not check out these articles below:
- PCOS and Bariatric Surgery
- Best Bariatric Surgery For Hiatal Hernia
- Bariatric Surgery and Diabetes
- Malabsorptive Bariatric Surgery
- Bariatric Surgery and Gallbladder
- Does Bariatric Surgery Cure Diabetes
Resources
Health Risks of Overweight and Obesity. (2023). NIH.
High Blood Pressure Risk Factors. (2024). CDC.
Transfer Addiction Following Bariatric Surgery. (2016). OAC.



What are your tips and tricks to post-bariatric success?